-
PDF
- Split View
-
Views
-
Cite
Cite
Yukihiro Tatekawa, A case of traumatic rupture of the urinary bladder due to a fall from a chair-style ski lift, Journal of Surgical Case Reports, Volume 2021, Issue 8, August 2021, rjab395, https://doi.org/10.1093/jscr/rjab395
Close - Share Icon Share
Abstract
We report our experience with an 8-year-old boy who incurred a traumatic rupture of the urinary bladder due to a fall from a chair-type ski lift. This boy felt like he needed to urinate before getting on the lift, but he did not do so. He was trembling from the sensation of needing to urinate and fell from the lift while it was at least 6 m in the air. He complained of abdominal pain, and on-site emergency physicians performed focused assessment with sonography for trauma, which showed fluid in the abdomen. He subsequently developed abdominal guarding. Enhanced abdominal computed tomography revealed a rupture of the urinary bladder. At laparotomy, two ruptures were seen along the dome of the bladder; the bladder wall was repaired in three layers. The patient was discharged with a cast on his foot for a fracture of the left heel bone on postoperative day 16.
INTRODUCTION
A report describing pediatric injuries resulting from falls from chair-style ski lifts notes that most such injuries occur in children who are 7 years of age and younger. The lower extremities are most likely to be involved in significant injuries resulting from such falls; femur fractures are most common [1].
Ruptures of the urinary bladder are categorized as either extraperitoneal or intraperitoneal, with treatments differing between the two types. Extraperitoneal injuries usually heal with urethral catheterization (bladder drainage) alone, while intraperitoneal injuries usually require a combination of surgical repair and bladder drainage [2–5]. Intraperitoneal ruptures usually occur when a full bladder is subjected to a compressive force applied to the lower abdomen. Extraperitoneal ruptures are usually associated with pelvic fractures: they may result from compressive forces on the pelvis, causing rupture of the anterior or lateral bladder wall, or they may result from direct penetration of the bladder by bony fragments. The empty bladder is well protected within the bony pelvis, but a full bladder may be distended to the level of the umbilicus, making it more vulnerable to injury. Bladder perforation or rupture is more likely if the bladder is full at the time of trauma [5]. In a clinical series of bladder perforations in children, the lesion typically occurred at the weakest part of the bladder: the dome.
CASE REPORT
An 8-year-old boy was at a ski resort for a competition. Although he felt like he needed to urinate before he got on the chair-style ski lift, he did not do so. He was on the lift by himself; he was wearing a helmet, but he did not lower the safety bar because he was used to riding this style of lift. He began to tremble with the sensation of holding in a full bladder and subsequently fell from the lift when it was at least 6 m in the air. There was no safety net below the chair, and he fell into an area of compressed snow.
He complained of abdominal pain, and abdominal distension was noted on examination. Emergency physicians from our hospital who happened to be on-site performed focused assessment with sonography for trauma (FAST), which showed fluid in the abdominal cavity. At this point, he was transported to our hospital by helicopter.
Upon arrival, the patient was alert and oriented but could not communicate very well because of abdominal pain. His heart rate was 106 beats/min, his blood pressure was 106/85 mm Hg and his respiratory rate was 24 breaths/min. His temperature was 37.1°C with 98% oxygen saturation. He was 122 cm tall and weighed 21 kg. He reported abdominal tenderness and left heel pain. He had a contusion on the right side of his forehead, but there were no contusions on the abdomen (Fig. 2a). He did display guarding on abdominal palpation. Laboratory evaluation showed a white blood cell count of 27.3/μl, an erythrocyte count of 516 × 104/μl, a C-reactive protein level of 0.04 mg/dl, total bilirubin of 0.5 mg/dl, aspartate aminotransferase (AST) of 155 IU/l, alanine aminotransferase (ALT) of 82 IU/l, amylase of 80 IU/l and creatine kinase of 416 IU/l (Table 1).
| WBC . | 27.3 × 103 /μ (4.0–9.0) . | BUN . | 37 mg/dl (8–21) . |
|---|---|---|---|
| RBC | 516 × 104 /μ (420–540) | CRE | 1.41 mg/dl (0.63–1.05) |
| Hb | 14.1 g/dl (13.0–18.0) | Na | 140 mEq/l (135–147) |
| Ht | 39.7 O/o (39.0–52.0) | K | 5.0 mEq/l (3.5–5.0) |
| Pits | 39.2 × 104 /μ (15.0–35.0) | CL | 104 mEq/l (98–110) |
| T-Bil | 0.5 mg/dl (0.3–1.4) | CRP | 0.04 mg/dl (<0.3) |
| AST | 155 IU/l (11–28) | ||
| ALT | 82 IU/l (6–30) | ||
| LD-IFCC | 605 U/l (124–222) | ||
| ALP-IFCC | 284 U/l (38–113) | ||
| CK | 416 IU/l (50–235) | ||
| AMY | 80 IU/l (43–116) |
| WBC . | 27.3 × 103 /μ (4.0–9.0) . | BUN . | 37 mg/dl (8–21) . |
|---|---|---|---|
| RBC | 516 × 104 /μ (420–540) | CRE | 1.41 mg/dl (0.63–1.05) |
| Hb | 14.1 g/dl (13.0–18.0) | Na | 140 mEq/l (135–147) |
| Ht | 39.7 O/o (39.0–52.0) | K | 5.0 mEq/l (3.5–5.0) |
| Pits | 39.2 × 104 /μ (15.0–35.0) | CL | 104 mEq/l (98–110) |
| T-Bil | 0.5 mg/dl (0.3–1.4) | CRP | 0.04 mg/dl (<0.3) |
| AST | 155 IU/l (11–28) | ||
| ALT | 82 IU/l (6–30) | ||
| LD-IFCC | 605 U/l (124–222) | ||
| ALP-IFCC | 284 U/l (38–113) | ||
| CK | 416 IU/l (50–235) | ||
| AMY | 80 IU/l (43–116) |
| WBC . | 27.3 × 103 /μ (4.0–9.0) . | BUN . | 37 mg/dl (8–21) . |
|---|---|---|---|
| RBC | 516 × 104 /μ (420–540) | CRE | 1.41 mg/dl (0.63–1.05) |
| Hb | 14.1 g/dl (13.0–18.0) | Na | 140 mEq/l (135–147) |
| Ht | 39.7 O/o (39.0–52.0) | K | 5.0 mEq/l (3.5–5.0) |
| Pits | 39.2 × 104 /μ (15.0–35.0) | CL | 104 mEq/l (98–110) |
| T-Bil | 0.5 mg/dl (0.3–1.4) | CRP | 0.04 mg/dl (<0.3) |
| AST | 155 IU/l (11–28) | ||
| ALT | 82 IU/l (6–30) | ||
| LD-IFCC | 605 U/l (124–222) | ||
| ALP-IFCC | 284 U/l (38–113) | ||
| CK | 416 IU/l (50–235) | ||
| AMY | 80 IU/l (43–116) |
| WBC . | 27.3 × 103 /μ (4.0–9.0) . | BUN . | 37 mg/dl (8–21) . |
|---|---|---|---|
| RBC | 516 × 104 /μ (420–540) | CRE | 1.41 mg/dl (0.63–1.05) |
| Hb | 14.1 g/dl (13.0–18.0) | Na | 140 mEq/l (135–147) |
| Ht | 39.7 O/o (39.0–52.0) | K | 5.0 mEq/l (3.5–5.0) |
| Pits | 39.2 × 104 /μ (15.0–35.0) | CL | 104 mEq/l (98–110) |
| T-Bil | 0.5 mg/dl (0.3–1.4) | CRP | 0.04 mg/dl (<0.3) |
| AST | 155 IU/l (11–28) | ||
| ALT | 82 IU/l (6–30) | ||
| LD-IFCC | 605 U/l (124–222) | ||
| ALP-IFCC | 284 U/l (38–113) | ||
| CK | 416 IU/l (50–235) | ||
| AMY | 80 IU/l (43–116) |
Enhanced abdominal computed tomography (CT) (Fig. 1a–d) and subsequent radiography (Fig. 1e) both revealed a rupture of the urinary bladder. Taken together with the laboratory results, our diagnosis was a bladder rupture without evidence of an underlying pelvic fracture.
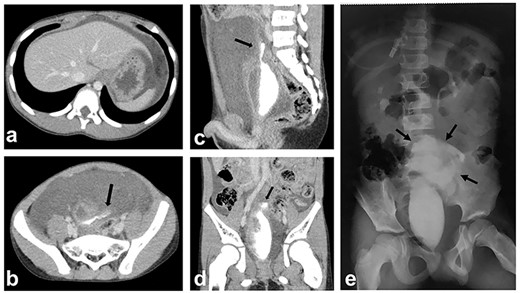
Enhanced CT and subsequent radiography; (a, b) enhanced CT shows a massive amount of intraperitoneal free fluid; (b–e) CT cystography and subsequent radiography show contrast material extravasating from the bladder; the contrast is confined to the intraperitoneal space (black arrows: extravasated contrast material).
We performed exploratory laparotomy through a lower abdominal midline incision. A massive amount of bloody ascites was noted in the abdominal cavity. Anterior to the bladder, there was a significant amount of edema, with bloody fluid noted between the membranes (Fig. 2b). The dome of the bladder was identified, and two ruptures were noted: one large and one small. The bladder wall at the rupture sites was repaired in three layers (Fig. 2c and d), and a urethral catheter was inserted for drainage. Inspection of the remainder of the abdominal cavity revealed no injuries.
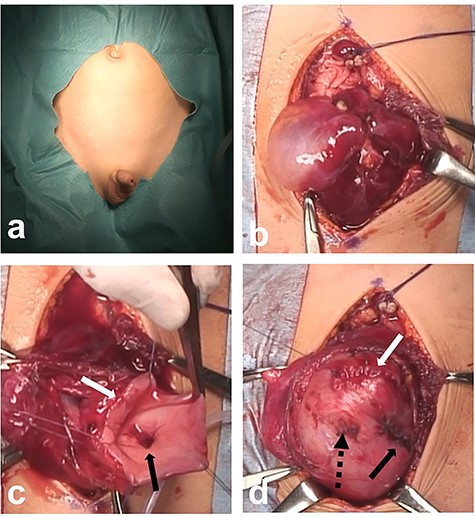
Intraoperative findings; (a) there are no visible contusions on the abdominal wall; (b) there is a large amount of bloody ascites in the abdominal cavity; massive edema and blood-tinged fluid are present anterior to the bladder; (c) two ruptures are visible along the dome of the bladder (white arrow: large rupture; black arrow: small rupture); (d) the bladder wall at the rupture sites is closed in three layers (white arrow: closure of large rupture; black arrow: closure of small rupture; black dotted arrow: stump of urachal remnant).
The day after surgery, the patient complained of left heel pain. Radiography revealed a fracture of the heel bone, and his left foot was set in a cast. On postoperative day 10, cystography performed through the urethral catheter showed no leakage from the injury sites. He was discharged on postoperative day 16 with a cast on his foot.
DISCUSSION
Bladder perforation or rupture must always be kept in mind when there is a pelvic injury associated with serious trauma. In adults with seat-belt induced bladder rupture, physical examination reveals large contusions over the lower abdomen [3]. Our patient had no such contusions, but FAST showed fluid in the abdominal cavity. It is important to note that FAST does not distinguish urine from blood, making this ultrasound modality nonspecific for intraperitoneal bleeding in patients with pelvic trauma. However, it is a useful modality for making initial judgments about the severity of trauma [6].
Enhanced CT of the abdomen, CT cystography and retrograde cystography are useful diagnostic modalities for rupture of the urinary bladder [2–6]. The use of CT cystography will reveal five types of bladder injury, allowing for prompt and effective treatment: contusion (Type 1), intraperitoneal rupture (Type 2), interstitial injury (Type 3), extraperitoneal rupture (Type 4) and combined intra- and extraperitoneal rupture (Type 5) [2]. In general, Type 2 and Type 5 injuries require surgical repair, while Type 1, Type 3 and Type 4 injuries are managed conservatively with urethral catheterization. However, there are many reports describing conservative treatment for Type 2 injuries [4].
Laparotomy with primary repair, with or without cystostomy, is the typical treatment for bladder injury [5]. Open surgery is necessary in patients with other injuries, but laparoscopic repair can be used in patients with isolated bladder injuries [7, 8]. In our patient, we could not be sure that he did not have intra-abdominal injuries, so we performed open surgery. Because our patient ended up having two discrete bladder rupture sites, laparotomy likely led to a better result than laparoscopic surgery would have.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No funding was used to support this manuscript.



