-
PDF
- Split View
-
Views
-
Cite
Cite
Chen Chuan Fang, Manjuvani Neerudu, Luis A Hernandez, Supradiaphragmatic accessory liver tissue mimicking pleural tumour: excision by transdiaphragmatic uniportal video-assisted thoracoscopic surgery (U-VATS), Journal of Surgical Case Reports, Volume 2021, Issue 8, August 2021, rjab338, https://doi.org/10.1093/jscr/rjab338
Close - Share Icon Share
Abstract
We describe a case of an extremely rare intrathoracic supradiaphragmatic accessory liver tissue that was excised via transdiaphragmatic uniportal video-assisted thoracoscopic surgery. The intrathoracic mass that was radiologically detected was found to be mimicking a pleural tumour because of its supradiaphragmatic location as well as the presence of a clear cleavage plane separating the mass and the liver completely. This, to our knowledge, is the first described case that was resected via transdiaphragmatic uniportal approach in the literature.
INTRODUCTION
The supradiaphragmatic location of accessory liver tissue is extremely rare. The clinical presentation is usually incidental and asymptomatic. In this article, we report a rare case of accessory liver tissue that was found and resected through the first ever reported transdiaphragmatic uniportal right video-assisted thoracoscopic surgery (U-VATS) in the literature.
CASE REPORT
A 65-year-old female, with a background history of breast cancer, presented with dysphagia. Physical examination was unremarkable. Computed tomography (CT) scan of neck and thorax (Fig. 1) revealed a 4.2 cm supradiaphragmatic pleural-based mass. This had gradually enlarged over the preceding 2 years (original size 1.7 cm) and was reported as suspicious of pleural fibroma. Subsequent positron emission tomography (PET) scan (Fig. 2) revealed a smooth, mildly avid peripheral/pleural-based 4.2 cm right lower lobe lung mass with a maximum standardized uptake value (SUVmax) of 4.3, contiguous with the right hemidiaphragm. Multidisciplinary team meetings were held, and the experts concluded that there was a clear cleavage plane between the slow growing mass and liver. The mass was thought to represent a solitary fibrous pleural tumour, and hence the decision for resection was made.
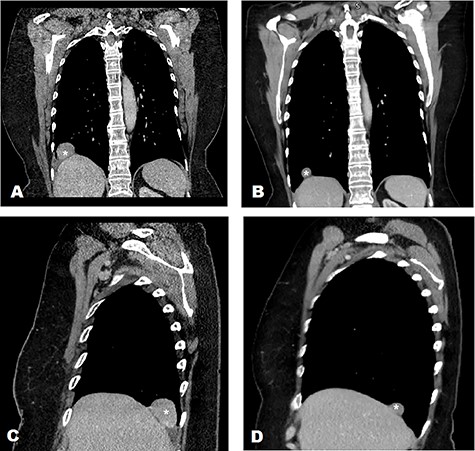
CT characterisation of supradiaphragmatic mass in 2 different views (mass marked with ‘*’) demonstrating a clear cleavage plane separating the mass and liver in 2020 and 2018. (A) CT scan of thorax in 2020—coronal view. (B) CT scan of thorax in 2018—coronal view. (C) CT scan of thorax in 2020—sagittal view of right hemithorax. (D) CT scan of thorax in 2018—sagittal view of right hemithorax.
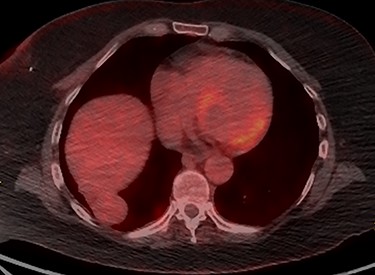
PET scan of Thorax demonstrating a smooth mildly avid peripheral/pleural-based right lower lobe mass with SUVmax of 4.3, which was contiguous with the right hemidiaphragm.
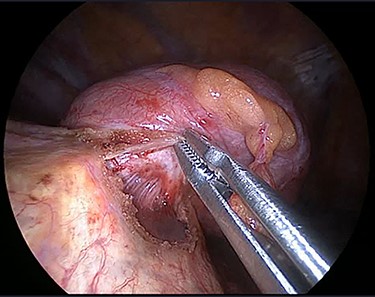
The operation was performed under general anaesthesia with the patient intubated using a double-lumen endotracheal tube. A 4 cm incision was made in the right sixth intercostal space in order to locate the mass. After the insertion of a 10 mm 30-degree thoracoscope, a rounded smooth-surfaced, broad necked mass attached to the right hemidiaphragm was visualized (Fig. 3). The decision to open the diaphragm was made. Further dissection and exploration with an energy device revealed that the mass which was bounded superiorly in the form of a pouch by the diaphragm and had arisen from the liver (Fig. 4). The mass was completely resected with HARMONIC ACE® +7 (Ethicon) after consulting with the hepatobiliary surgeon who felt there was a clear cleavage plane between the mass and liver. The exposed area of liver was covered with Floseal®(Baxter) and TachoSil®(Takeda). The diaphragmatic defect (Fig. 5) was closed in a single layer with 10 simple interrupted silk sutures (Fig. 6). The remainder of the surgery was uncomplicated, and the patient was discharged home on the second postoperative day. Subsequent histology findings reported the mass as benign (accessory) hepatic tissue (Fig. 7).

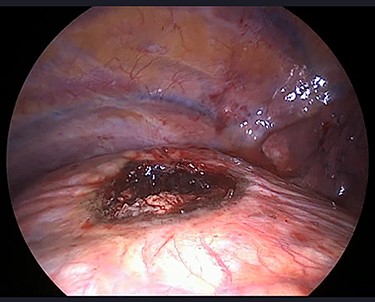
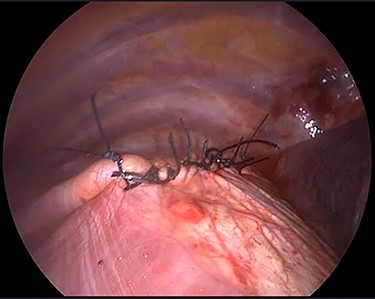
Diaphragmatic defect was closed in a single layer with simple interrupted stitches.
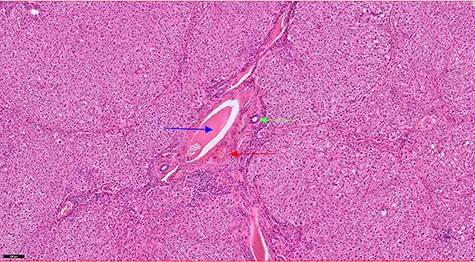
Haematoxylin and eosin staining section showing a portal tract containing a portal vein (blue arrow), hepatic artery (red arrow) and a bile duct (green arrow).
DISCUSSION
A supradiaphragmatic liver mass is very rare [1], and the diagnosis of such an unusual anomaly is difficult. In this study, we report a case of intrathoracic supradiaphragmatic accessory liver tissue that was presumed to be a pleural-based tumour preoperatively. The CT scan of the chest had clearly demonstrated a plane that separated the mass and liver. The possibility of a liver herniation, on the other hand, had been ruled out because of the fact that patient had no trauma history and the finding of an intact diaphragm during thoracoscopic exploration.
A total of 25 intrathoracic supradiaphragmatic liver case reports (in the absence of diaphragmatic herniation) were presented in the literature in the past 64 years [1, 2]. Out of the 25 cases, 17 of these masses were resected via thoracotomy, whereas 7 were excised via other approaches. One of the most recently published cases reported a uniportal VATS frozen section rather than a full resection. To the best of our knowledge, this is the first ever described case of a rare supradiaphragmatic intrathoracic accessory liver tissue, which was resected completely via transdiaphragmatic U-VATS in the literature. Of those cases reported in the literature, almost all were misdiagnosed preoperatively. These masses most commonly mimic a pulmonary tumour and occasionally are reported as pulmonary sequestration or hydatid cyst.
The first uniportal VATS lobectomy was reported by Gonzalez-Rivas et al. in 2011 [3]. Uniportal VATS has been reported to decrease postoperative pain and shorten hospital stay, thereby promoting more rapid recovery and providing superior cosmetic results when compared with traditional three-port VATS [4]. Uniportal VATS is also advantageous to the surgeon because it provides a more anatomic and direct view of the target tissues.
CONCLUSION
Supradiaphragmatic accessory liver tissue is seen very rarely and can be overlooked on a radiological examination. It should be considered in the differential diagnosis of right sided supradiaphragmatic masses. A transdiaphragmatic uniportal VATS approach resection can be effectively employed for the diagnosis and treatment of such asymptomatic accessory liver tissue with unremarkable outcomes.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
The authors received no specific funding for this work.



