-
PDF
- Split View
-
Views
-
Cite
Cite
Akiharu Kimura, Nobuhiro Morinaga, Kohei Tajima, Kyoichi Ogata, Hiroyuki Kato, Makoto Sohda, Ken Shirabe, Hiroshi Saeki, Colon angiolipoma with intussusception resected by laparoscopy-assisted surgery: a case report, Journal of Surgical Case Reports, Volume 2021, Issue 8, August 2021, rjab329, https://doi.org/10.1093/jscr/rjab329
Close - Share Icon Share
Abstract
Angiolipomas are benign mesenchymal tumors that often occur under the skin of the upper extremity or thoracic and abdominal walls. Angiolipomas of the digestive tract are rare. Here, we describe a case of transverse colon angiolipoma with intussusception resected by laparoscopy-assisted surgery. A 50-year-old woman visited a family hospital with complaints of left lower abdominal pain and bloody stool. Colonoscopy revealed a submucosal tumor in her left colon. She was referred to our hospital for further examination. Computed tomography revealed a low-density tumor with intussusception in the left transverse colon. Elective surgery was planned for this patient because there were no alarming symptoms such as ileus or obstruction. Laparoscopy-assisted surgery and partial resection of the left transverse colon were performed. The histopathological diagnosis was angiolipoma of the colon. Angiolipomas are benign mesenchymal tumors that rarely occur in the digestive tract. Thus, accurate preoperative diagnosis is difficult.
INTRODUCTION
Common nonepithelial benign tumors in the colon are lipomas and leiomyomas, whereas malignant tumors include lymphomas or leiomyosarcomas. Angiolipomas often occur under the skin of the upper extremity or thoracic and abdominal walls. However, these rarely occur in the digestive tract. Herein, we report a case of transverse colon angiolipoma with intussusception resected by laparoscopy-assisted surgery.
CASE REPORTS
A 50-year-old woman visited a family hospital with complaints of left lower abdominal pain and bloody stool. She had no relevant past medical history or family history. She underwent colonoscopy, and a submucosal tumor was detected in her colon. She was referred to our hospital for further testing and treatment. Colonoscopy was performed, and an ulcerating submucosal tumor with necrosis at the surface was detected in the colon 40 cm from anal verge (Fig. 1). There were no other abnormal lesions in her colon. Histopathological examination of biopsy samples of the tumor comprised only exudate and no cellular components.
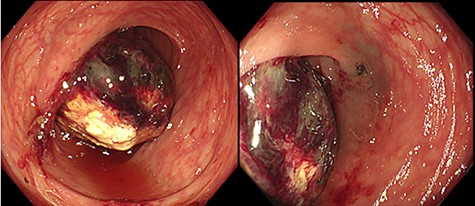
Colonoscopy findings: a submucosal tumor with ulceration and necrosis at the surface was detected in the colon 40 cm from anal verge. There were no other abnormal lesions in her colon.
Her body height was 158.0 cm and her weight was 51.0 kg. Her abdomen was soft and without tenderness. There were no palpable tumors. Laboratory tests showed a white blood cell count of 5.3 × 109/L, a red blood cell count of 4.72 × 1012/L, and a hemoglobin level of 14.0 g/dl. Tumor markers such as carbohydrate antigen 19-9 and carcinoembryonic antigen were within normal levels. An abdominal enhanced computed tomography (CT) imaging performed on her first visit revealed a 3.5-cm low-density and low-enhanced tumor with intussusception in the left side of her colon. No swollen lymph nodes around the tumor were detected, and there was no evidence of any tumor invasion or metastasis (Fig. 2). We performed elective surgery for this patient because she had no alarming symptoms. Two weeks after her first visit, the patient was reexamined via abdominal CT scan. There were no findings of intussusception, and the same low-density tumor was found in her left transverse colon near the splenic flexure. Based on the above results, it is likely that the submucosal tumor of the left transverse colon caused intussusception.
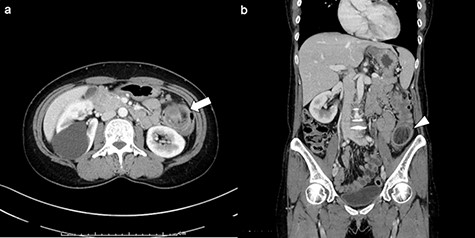
Enhanced CT imaging of abdomen: (a) axial view. Three-layer like appearance indicating the intussusception was found in left side of colon (arrow). (b) Coronal view. The lead mass was detected as a 3.5-cm low-density tumor (arrowhead).
At first, we considered that this was a submucosal tumor, with our differential diagnoses being lipoma or gastrointestinal stromal tumor with necrosis according to a low-density and low-enhanced tumor from CT findings. Colon cancer could not be excluded. There was no progression of her abdominal symptoms, and elective surgery was performed 16 days after her first visit. Under general anesthesia, we found a tumor in the left transverse colon laparoscopically (Fig. 3a). The tumor had good mobility with no evidence of invasion, lymph node metastasis or peritoneal dissemination. Partial resection of the left transverse colon was performed. The main feeders of the tumor were branches of the left colic artery, and it was cut after ligation (Fig. 3b). The intestinal tracts were anastomosed via functional end-to-end anastomosis. The operation time was 162 min and blood loss was 20 ml.
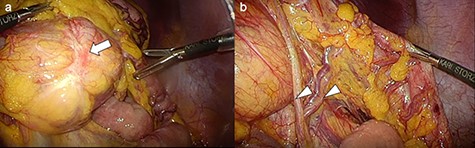
Operative findings: (a) A tumor was detected in the left transverse colon (arrow). The tumor had good mobility with no evidence of invasion to the surrounding tissue. (b) The main feeders of the tumor were branches of the left colic artery (arrowhead).
A submucosal tumor with a diameter of 3.0 × 2.5 cm was resected. Pathological findings revealed outgrowth of mature fat tissues and vessel tissues. On immunohistochemical staining, the specimen was Berlin blue positive for both tissue, CD34 positive for vessel tissue, desmin negative, α-smooth muscle actin positive for vessel tissue, S-100 negative and CD68 negative. There was no evidence of tumor cells in the lymph node tissue. The final pathological diagnosis was angiolipoma of the transverse colon (Fig. 4). The patient had a good postoperative course and started eating meals on the 4th day postoperatively. She was discharged from the hospital on the 13th day postoperatively. There was no evidence of recurrence at the 1-year follow-up.
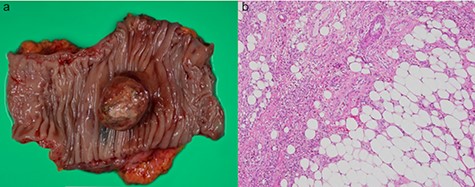
Resected specimen and pathological findings: (a) Resected specimen with a tumor size of 3.0 × 2.5 cm in diameter. The surface of tumor was relatively smooth, similar to that of a submucosal tumor. (b) Pathological findings: The outgrowth of mature fat tissue and vessel tissue were found in the tumor tissue (Hematoxylin & Eosin, ×400).
| Author . | Year . | Gender . | Age . | Location . | Tumor size (mm) . | Symptoms . | Intussusception . | Treatment . |
|---|---|---|---|---|---|---|---|---|
| Vandamme | 1964 | Male | 43 | S | 40 | Bloody stool | No | Partial resection |
| Okuyama | 2002 | Male | 49 | S | 65 | Fecal occult blood | No | Endoscopic resection |
| Mohl | 2004 | Male | 66 | Unknown | Unknown | None | No | Endoscopic resection |
| Chen | 2005 | Male | 70 | T | 50 | Bloody stool, abdominal distention, abdominal pain | No | Partial resection |
| Oishi | 2009 | Male | 51 | D | 57 | Abdominal pain | No | Partial resection |
| Lu | 2011 | Male | 75 | A | 70 | Bloody stool, diarrhea, abdominal pain | No | Partial resection |
| Demir | 2011 | Male | 70 | S | unknown | Bloody stool | No | Sigmoidectomy |
| Grasso | 2012 | Female | 54 | D | unknown | Bloody stool, nausea, abdominal pain | Yes | Left hemicolectomy (emergency) |
| Molinares | 2012 | Male | 72 | A | 63 | Diarrhea, abdominal pain | No | Partial resection |
| Wang | 2013 | Male | 58 | D | 80 | Abdominal discomfort, bloody stool | Yes | Partial resection (emergency) |
| Park | 2014 | Male | 67 | S | 20 | Abdominal pain, indigestion, decreased stool caliber | No | Endoscopic resection |
| Hang | 2014 | Female | 48 | T | 50 | Altered bowel habit | No | Partial resection |
| Foltz | 2015 | Male | 75 | D | 49 | Bloody stool, constipation, diarrhea, abdominal pain | No | Endoscopic resection |
| Nissen | 2017 | Female | 41 | A | 60 | Abdominal pain | Yes | Robotic-assisted right hemicolectomy |
| Our Case | 2019 | Female | 50 | T | 30 | Bloody stool, abdominal pain | Yes | Laparoscopic partial resection |
| Author . | Year . | Gender . | Age . | Location . | Tumor size (mm) . | Symptoms . | Intussusception . | Treatment . |
|---|---|---|---|---|---|---|---|---|
| Vandamme | 1964 | Male | 43 | S | 40 | Bloody stool | No | Partial resection |
| Okuyama | 2002 | Male | 49 | S | 65 | Fecal occult blood | No | Endoscopic resection |
| Mohl | 2004 | Male | 66 | Unknown | Unknown | None | No | Endoscopic resection |
| Chen | 2005 | Male | 70 | T | 50 | Bloody stool, abdominal distention, abdominal pain | No | Partial resection |
| Oishi | 2009 | Male | 51 | D | 57 | Abdominal pain | No | Partial resection |
| Lu | 2011 | Male | 75 | A | 70 | Bloody stool, diarrhea, abdominal pain | No | Partial resection |
| Demir | 2011 | Male | 70 | S | unknown | Bloody stool | No | Sigmoidectomy |
| Grasso | 2012 | Female | 54 | D | unknown | Bloody stool, nausea, abdominal pain | Yes | Left hemicolectomy (emergency) |
| Molinares | 2012 | Male | 72 | A | 63 | Diarrhea, abdominal pain | No | Partial resection |
| Wang | 2013 | Male | 58 | D | 80 | Abdominal discomfort, bloody stool | Yes | Partial resection (emergency) |
| Park | 2014 | Male | 67 | S | 20 | Abdominal pain, indigestion, decreased stool caliber | No | Endoscopic resection |
| Hang | 2014 | Female | 48 | T | 50 | Altered bowel habit | No | Partial resection |
| Foltz | 2015 | Male | 75 | D | 49 | Bloody stool, constipation, diarrhea, abdominal pain | No | Endoscopic resection |
| Nissen | 2017 | Female | 41 | A | 60 | Abdominal pain | Yes | Robotic-assisted right hemicolectomy |
| Our Case | 2019 | Female | 50 | T | 30 | Bloody stool, abdominal pain | Yes | Laparoscopic partial resection |
A: ascending colon, T: transverse colon, D: descending colon, S: sigmoid colon.
| Author . | Year . | Gender . | Age . | Location . | Tumor size (mm) . | Symptoms . | Intussusception . | Treatment . |
|---|---|---|---|---|---|---|---|---|
| Vandamme | 1964 | Male | 43 | S | 40 | Bloody stool | No | Partial resection |
| Okuyama | 2002 | Male | 49 | S | 65 | Fecal occult blood | No | Endoscopic resection |
| Mohl | 2004 | Male | 66 | Unknown | Unknown | None | No | Endoscopic resection |
| Chen | 2005 | Male | 70 | T | 50 | Bloody stool, abdominal distention, abdominal pain | No | Partial resection |
| Oishi | 2009 | Male | 51 | D | 57 | Abdominal pain | No | Partial resection |
| Lu | 2011 | Male | 75 | A | 70 | Bloody stool, diarrhea, abdominal pain | No | Partial resection |
| Demir | 2011 | Male | 70 | S | unknown | Bloody stool | No | Sigmoidectomy |
| Grasso | 2012 | Female | 54 | D | unknown | Bloody stool, nausea, abdominal pain | Yes | Left hemicolectomy (emergency) |
| Molinares | 2012 | Male | 72 | A | 63 | Diarrhea, abdominal pain | No | Partial resection |
| Wang | 2013 | Male | 58 | D | 80 | Abdominal discomfort, bloody stool | Yes | Partial resection (emergency) |
| Park | 2014 | Male | 67 | S | 20 | Abdominal pain, indigestion, decreased stool caliber | No | Endoscopic resection |
| Hang | 2014 | Female | 48 | T | 50 | Altered bowel habit | No | Partial resection |
| Foltz | 2015 | Male | 75 | D | 49 | Bloody stool, constipation, diarrhea, abdominal pain | No | Endoscopic resection |
| Nissen | 2017 | Female | 41 | A | 60 | Abdominal pain | Yes | Robotic-assisted right hemicolectomy |
| Our Case | 2019 | Female | 50 | T | 30 | Bloody stool, abdominal pain | Yes | Laparoscopic partial resection |
| Author . | Year . | Gender . | Age . | Location . | Tumor size (mm) . | Symptoms . | Intussusception . | Treatment . |
|---|---|---|---|---|---|---|---|---|
| Vandamme | 1964 | Male | 43 | S | 40 | Bloody stool | No | Partial resection |
| Okuyama | 2002 | Male | 49 | S | 65 | Fecal occult blood | No | Endoscopic resection |
| Mohl | 2004 | Male | 66 | Unknown | Unknown | None | No | Endoscopic resection |
| Chen | 2005 | Male | 70 | T | 50 | Bloody stool, abdominal distention, abdominal pain | No | Partial resection |
| Oishi | 2009 | Male | 51 | D | 57 | Abdominal pain | No | Partial resection |
| Lu | 2011 | Male | 75 | A | 70 | Bloody stool, diarrhea, abdominal pain | No | Partial resection |
| Demir | 2011 | Male | 70 | S | unknown | Bloody stool | No | Sigmoidectomy |
| Grasso | 2012 | Female | 54 | D | unknown | Bloody stool, nausea, abdominal pain | Yes | Left hemicolectomy (emergency) |
| Molinares | 2012 | Male | 72 | A | 63 | Diarrhea, abdominal pain | No | Partial resection |
| Wang | 2013 | Male | 58 | D | 80 | Abdominal discomfort, bloody stool | Yes | Partial resection (emergency) |
| Park | 2014 | Male | 67 | S | 20 | Abdominal pain, indigestion, decreased stool caliber | No | Endoscopic resection |
| Hang | 2014 | Female | 48 | T | 50 | Altered bowel habit | No | Partial resection |
| Foltz | 2015 | Male | 75 | D | 49 | Bloody stool, constipation, diarrhea, abdominal pain | No | Endoscopic resection |
| Nissen | 2017 | Female | 41 | A | 60 | Abdominal pain | Yes | Robotic-assisted right hemicolectomy |
| Our Case | 2019 | Female | 50 | T | 30 | Bloody stool, abdominal pain | Yes | Laparoscopic partial resection |
A: ascending colon, T: transverse colon, D: descending colon, S: sigmoid colon.
DISCUSSION
Angiolipomas were first reported by Bowen in 1912 [1]. In 1960, Howard reported that the clinicopathological features of angiolipomas were different from those of lipomas in that they often occur under the skin of the upper extremity or thoracic and abdominal walls [2]. Angiolipomas most commonly occurs in men in their late teens and ~25 years old [3]. Pathologically, it is characterized by a capsule and clear boundaries. They are benign tumors containing mature fat tissue and blood capillaries and rarely undergo malignant transformation [2]. They are classified as either lipoma type or hemangioma type depending on the proportion of fat and vessels [4–6].
Angiolipomas rarely occur in the digestive tract. In a literature review, we found only 35 cases of angiolipoma occurring in the digestive tract: 1 of esophagus [7]; 6 of the stomach [8–11]; 3 of the duodenum [12–14]; 6 of the small intestine [15–20]; 3 of the ileocecal junction [21–23]; 14 of the colon [3, 4, 13, 14, 24–33] and 2 of the rectum [5, 6].
The known cases of colon angiolipoma, including our case, are presented in Table 1. There were 11 males and 4 females. The mean age was 59.3 (range: 41–75) years. Regarding tumor location, three were in the ascending colon, three in the transverse colon, four in the descending colon, and four in the sigmoid colon; in one case, the location was unknown. The mean tumor size was 52.8 (range: 20–80) mm. All cases involved a single submucosal tumor. Apart from two cases, all other cases had symptoms such as bloody stool, abdominal pain or distention, constipation and diarrhea. Intussusception of the colon was found in four cases, including our case. Emergency operation was performed for two patients with intussusception. Surgical resection (i.e. partial resection or hemicolectomy) was performed for 11 cases; endoscopic resection was performed for four cases; this information. Colon angiolipoma with intussusception is rare and was only reported in three other studies apart from our case [4, 30, 33]. Kacar et al. [5] reported that the level of urgency was an important factor when choosing the optimal treatment. In cases with intussusception, acute bleeding, or obstruction, emergency surgery was generally suggested instead of further auxiliary examination. In our case, we chose elective surgery because the patient had no abdominal symptoms during observation. Consequently, we could safely perform laparoscopy-assisted surgery. Siamionava et al. [34] reported a case of colon lipoma with several episodes of bowel obstruction, in which elective surgery was performed after conservative treatment. Nissen et al. [33] reported an angiolipoma of the ascending colon with intussusception, in which elective robotic-assisted surgery was performed. Emergency operation for colon intussusception might not be necessary if patients do not have symptoms such as abdominal pain owing to obstruction or severe melena.
Angiolipomas of the digestive tract often grow as submucosal tumors with pedicles or subpedicles [29]. Angiolipomas have a few clinical features that differentiate them from other submucosal tumors; these tend to be less yellowish and harder than lipomas. Barium enema shows filling defect of the digestive tract and describes an elevated lesion with a smooth surface and clear edges. However, these findings are often similar to those of other submucosal tumors [3, 4, 18]. Colonoscopy findings show a submucosal tumor covered with normal mucosa, similar to other submucosal tumors. Magnetic resonance imaging shows central high signal intensity and peripheral isosignal intensity on T1-weighted in-phase images [18]. It is difficult to differentiate angiolipomas from other submucosal tumors such as lipoma via imaging. Moreover, it is difficult to collect adequate samples via endoscopic biopsy similar to that in our case. A pathological diagnosis with a resected specimen is necessary to make a definite diagnosis. Sasaki et al. [35] evaluated the usefulness of endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) for submucosal and extrinsic masses of the colon and rectum. They reported that the overall rate of detection of malignant and benign masses was 95.5% for EUS-FNA. A preoperative diagnosis could have been made via EUS-FNA in our case, but we were unable to do so because our institution did not have the equipment to perform this.
The treatment of colon angiolipoma requires tumor resection, and the methods of resection differ depending on the tumor type. Small pedunculated tumors can be removed via colonoscopy [14, 25], whereas large tumors or broad-based polyps need surgical resection [20]. Partial resection of the colon including the tumor is an adaptable modality for treatment [22, 25]. If a tumor is completely resected, the prognosis is good. However, if resection is inadequate, there is a high probability of recurrence [6, 19]. Recently, some patients with colon angiolipoma underwent minimally invasive procedures such as laparoscopic resection. Kato et al. [22] reported an angiolipoma in the ileocecal junction, which was resected via laparoscopy-assisted ileocecostomy, and the patient showed no signs or symptoms of recurrence at 5 years of follow-up. Ishizuka et al. [6] reported a case of rectal angiolipoma resected via a transanal approach. Wang et al. [4] performed rapid pathologic diagnosis during surgery for a colon angiolipoma and avoided unnecessary radical resection. In our case, we did not perform a rapid pathologic diagnosis during operation, and the branch of the left colic artery was cut after ligation. The blood loss was low, and we performed a minimally invasive laparoscopy-assisted resection.
CONCLUSION
We encountered a case of transverse colon angiolipoma with intussusception resected via laparoscopy-assisted surgery. Angiolipomas of the digestive tract are rare, and it is difficult to make a correct preoperative diagnosis. If the patients are asymptomatic when there are findings of intussusception, then elective laparoscopy-assisted resection might be a choice of minimally invasive treatment.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The patient has provided permission to publish this case report and her identity has been protected.
AUTHORS' CONTRIBUTIONS
AK is the first author and the corresponding author of this manuscript. All authors contributed in performing the surgeries and collecting and analyzing data. All authors read and approved the final manuscript.
ACKNOWLEDGMENTS
We thank Edanz Group (https://en-author-services.edanz.com/ac) for editing a draft of this manuscript.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
This study received no funding.



