-
PDF
- Split View
-
Views
-
Cite
Cite
Chen-Yueh Wen, Kai-Hung Ho, Meng-Yu Wu, Jen-Tai Lin, Chia-Cheng Yu, Yin-Shen Chen, Novel approach to removing a steel bar extending from the scrotum to anterior abdominal wall: a case report, Journal of Surgical Case Reports, Volume 2021, Issue 7, July 2021, rjab330, https://doi.org/10.1093/jscr/rjab330
Close - Share Icon Share
Abstract
Foreign body penetration from the scrotum is not rare. If a large and sharp foreign body pierces through an existing wound, it likely must be extended to improve exposure. Therefore, many traumatologists attempt to minimize the surgical wound caused by the removal of the foreign body. We describe a case of a foreign object penetrating from the scrotum to anterior abdominal wall. Our novel surgical approach is safe and feasible to use and provides minimal scarring, thereby allowing rapid recovery.
INTRODUCTION
Foreign body penetration from the scrotum is not rare. If a large and sharp foreign body pierces through an existing wound, it likely must be extended to improve exposure [1]. Therefore, many traumatologists attempt to minimize the surgical wound caused by the removal of the foreign body. Radiological studies provide three dimensions location information and guide the placement of the incision anywhere along the foreign body, thus preserving the anatomic structure of the affected area and reducing the severity of surgical wounds [2]. To our knowledge, ours is the first case report in which a foreign body extending from the scrotum to the anterior abdominal wall is removed through a novel approach where two skip incisions are made.
CASE PRESENTATION
A 55-year-old man presented with traumatic injury due to a foreign object penetrating his scrotum when he slipped and fell. This foreign object was a steel bar that penetrated his left scrotum and extended to his abdomen (Fig. 1A and B). Upon physical examination, his blood pressure, heart rate and Glasgow Coma Score were 122/75 mmHg, 131 beats/min and E4V5M6, respectively. Laboratory investigation indicated leukocytosis (10 700/ul, normal range: 3900–10 400/ul) and no anemia. A portable radiography reading showed that the penetration extended from the left scrotum to the right abdomen but indicated no injury to the pelvic bone or spine (Fig. 1C). An abdominal computed tomography (CT) scan demonstrated that the penetration extended from the left scrotum to the right anterior abdomen wall (Fig. 2). Emergency surgical removal of the steel bar was performed for debridement and repair. First, two skip incisions were created on the tip and middle portion of steel bar. Subsequently, curved Kelly forceps were used for guiding with a Jackson-Pratt (JP) drain to prevent wrong placing tract and gently removed the steel bar (Figs 3 and 4). Thereafter, the wound was irrigated with copious normal saline, and the bleeders were then checked. No additional injury was found in the peritoneum, testes and spermatic cord. Blood loss was minimal (<5 ml). No immediate intra-operative complications were noted. The patient received intravenous broad-spectrum antibiotics after surgery and was discharged on the fifth day after the operation with fair convalescence.
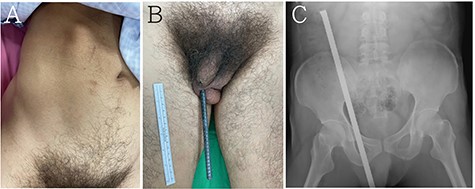
(A, B) a steel bar penetrated his left scrotum and extended to his abdomen. (C) Abdominal radiography showed the penetration extended from the left scrotum to the right abdomen but indicated no injury to the pelvic bone or spine.
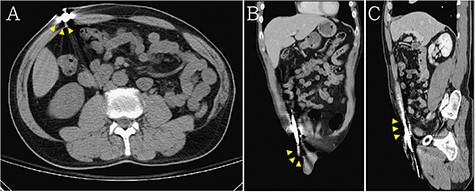
Abdominal CT demonstrated that the penetration extended from the left scrotum to the right anterior abdomen wall (the steel bar: yellow arrow head) in (A) axial view, (B) coronal view and (C) sagittal view.
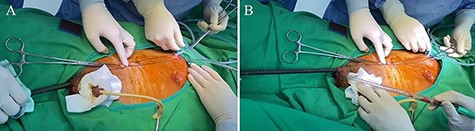
(A, B) curved Kelly forceps along with JP drain guided to remove the steel bar simultaneously and prevented from wrong placing tract.
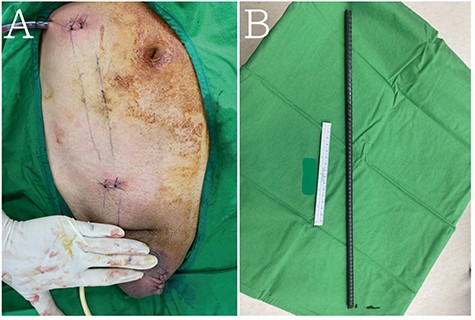
(A) Two skip incisions were created to remove (B) the steel bar.
DISCUSSION
Pre-peritoneal injury involving metallic foreign bodies presents many challenges. Clinical image diagnosis of peritoneal and testicular integrity may be difficult because metallic foreign bodies have a high atomic number and thus interfere with the interpretation of CT readings for adjacent organs [3]. In our case, we could not determine whether any damage was caused to the genital organs because the steel bar induced noise in the signal. Considering the size and location of this foreign body, the patient required a trip to the operating theater and consultation with a urologist regarding its removal.
Skip incisions have been applied in some surgical procedures, such as minimally invasive plate osteosynthesis [4] and minimally invasive transforaminal lumbar interbody fusion [5]. Such incisions have the advantages of being less invasive and having better cosmesis. We retrieved the steel bar from the scrotum in our patient by making two skip incisions. Contrary to expectations, this approach was not much more difficult than conventional surgery. One challenge of skip incisions and the removal of foreign bodies is the determination of whether any injury to the vessels has occurred. Bleeding is difficult to control if the gonadal and inferior epigastric vessels are not visible. The surgical wound should be extended if bleeding becomes uncontrollable. Fortunately, we guided our approach using curved Kelly forceps with a JP drain to smoothly remove the steel bar without uncontrollable bleeding. The method of creating skip incisions is also worth considering. Because we observed that the protrusion of the distal end of steel bar did not penetrate the skin, we created the first surgical wound at the steel bar’s distal end. In addition, another surgical wound was made to secure the steel bar intact without fracture. This approach was more attractive because the wound recovered quickly with few unsightly scars remaining.
Foreign bodies are usually unsterile and carry many unknown microorganisms that can induce sepsis after the foreign body has been removed. Previous studies have reported that infection can be caused by invisible metallic briquette that is retained in the body, highlighting the necessity of rapid removal and administration of antibiotic therapy [1, 6]. In the current case, we used an intravenous antibiotic regimen of cefazolin, gentamicin and metronidazole for empirical coverage. The patient had no fever during hospitalization, and his white blood cell count returned to normal (8290/ul) on the first day after the operation.
In summary, we report a rare case of scrotum trauma caused by penetration of a large and sharp metallic foreign body without injury to the testes, spermatic cord or abdominal cavity. Our novel approach for removing the foreign body is safe and feasible. It has the benefits of short operation time, minimal invasiveness, quick recovery and minimal scarring.
CONFLICT OF INTEREST STATEMENT
None to declare.



