-
PDF
- Split View
-
Views
-
Cite
Cite
Sofia El Akroud, Yao Christian Hugues Dokponou, Mamoune El Mostarchid, Hafsa Chahdi, Abad Cherif El Asri, Miloudi Gazzaz, Management and positive outcome of skull-base ossifying fibroma: a case report, Journal of Surgical Case Reports, Volume 2021, Issue 7, July 2021, rjab304, https://doi.org/10.1093/jscr/rjab304
Close - Share Icon Share
Abstract
The ossifying fibroma is a benign fibro-osseous tumor rarely affecting the skull base. The incidence of ossifying fibroma itself is uncommon. It is considered to be an aggressive and fast-growing bone lesion. Early detection and complete surgical removal are essential to deal with its aggressive nature and recurrence. We report a case of a 20-year-old man admitted for the management of ossifying fibroma of the orbital roof extending inside the orbit mimicking meningioma and revealed by a progressive proptosis and headache. The patient underwent surgery for the subtotal removal of the tumor with its frontal infiltration with a good outcome. All meningiomas like tumors are not meningiomas and other tumors such as ossifying fibroma might be mistaken for meningioma and even get confirmation from the pathological anatomy study. Need be for these tumors to be looked at more closely for better therapeutic decision-making.
INTRODUCTION
Fibro-osseous lesions are a diverse group of lesions characterized by a process leading to the replacement of normal bone by fibrous tissue, collagen tissue containing newly formed mineralized tissue, giant cells and blood vessels. They represent a diagnostic challenge for the pathologist because histologically, they are not easily distinguishable and might be mistaken for meningioma [1]. The ossifying fibromas are benign but potentially locally aggressive fibro-osseous lesions, predominantly originating in the paranasal sinuses. Juvenile psammomatoid ossifying fibroma (JPOF) is a variant of ossifying fibroma. According to the 2005 WHO classification of odontogenic tumors, JPOF is one of the most frequent pathologies, of the craniofacial skeleton. Intracranial extension, although rare, sometimes occurs [2]. They have been reported to rarely occur in the skull base, orbital roof in particular [3]. Total gross tumor resection is the gold standard for managing to avoid multiple recurrences by preserving a patient’s quality of life. We report a clinical case of an ossifying fibroma extending to the orbital roof and the orbit, mimicking meningioma and revealed by a right-sided proptosis and headache. The patient underwent surgery for subtotal removal of the tumor with frontal infiltration followed by frontal bone cranioplasty a year after surgery.
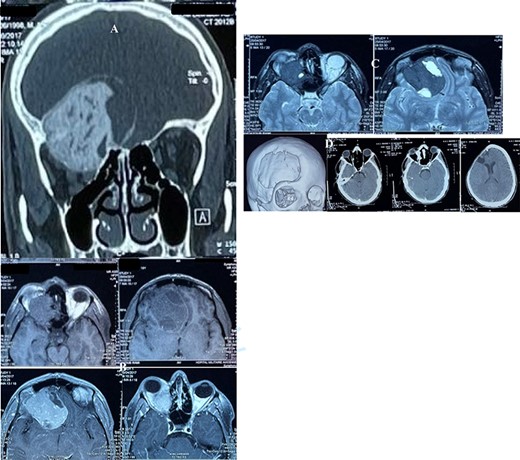
(A) CT scan, bone window, coronal reconstruction, showing well-defined ground glass lesion lying on the orbital roof invading the orbit and above the roof. (B) T1 weighted MRI images showing an expansile, heterogeneous and cystic lesion involving the orbital roof and invading the orbit below and the cranium above, with an enhancing after injection. (C) T2 weighted MRI images: the tumor is of a low intensity, whereas the cystic parts is hyperintense. (D) Postoperative CT scan, showing successful resection of the majority of the lesion.
CASE REPORT
A 20-years-old male with no significant medical history presented to our department with a chief complaint of right eye proptosis of progressive appearance in the past 4 months without any disturbances of vision or diplopia. The patient denied any history of trauma or medication before the symptoms. His family history was unremarkable.
On examination, the patient was alert with a Glasgow coma scale of 15/15, in good general status, without fever. There was no sensory or motor palsy. The right eye proptosis was unilateral, it was non-axial, painless and hard on palpation with a normal conjugate ocular motion. With 9/10 visual acuity in each eye, the ophthalmoscopic examination revealed a grade 2 papilledema on the right side. The laboratory blood sample test was normal.
The cerebral CT scan revealed a large heterogeneous mass with ground glass appearance, which lies in orbit extending to the roof of the right orbit and above the roof, associated with significant bony erosion (Fig. 1A). The lesion was reported radiologically as consistent with skull-base meningioma and less likely ossifying fibroma. On magnetic resonance imaging (MRI), the lesion was delineated more in detail (Fig. 1B–C).
He underwent surgery 3 days later, for the removal of the tumor with resection of the involved frontal bone. The tumor was exposed, grayish and cartilaginous in consistency, and we performed a subtotal removal, the debulking by piecemeal resection. The postoperative period was unremarkable, and the patient was discharged 8 days after surgery (Fig. 1D). The cranioplasty was done successfully a year after his surgical procedure with a good outcome. The sample was sent to the histopathology for analysis and confirmed the lesion to be an ossifying fibroma with fibrous dysplasia and irregularly shaped bony trabeculae embedded within a moderately cellular fibrous stroma (Fig. 2).
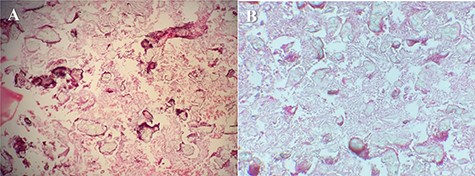
(A) Irregularly shaped bony trabeculae embedded within a moderately cellular fibrous stroma. Artifactual separation of the bony elements from the surrounding fibrous tissue also is seen (H&E, ×100). (B) Fibrous dysplasia.
DISCUSSION
The ossifying fibroma is a rare benign fibro-osseous lesion. These tumors typically arise in the craniofacial skeleton, mostly in the mandible, but other uncommon locations as the skull base have been reported. Rahmani et al. reported that only 70 cases of JPOF were registered during the last 36 years [4]. These lesions display male predilection and usually develop during the first and the second decade of life [5]. Exactly the case of our patient aged 19.
Based on the symptoms and the site of lesion and radiographic findings, a provisional diagnosis can be thought to be another kind of tumor, such as fibrous dysplasia or psammomatoid meningioma, which are the main differential diagnoses [6]. Since the diagnosis is hard to make due to the low prevalence, it could only occur if the correlation between clinical symptoms, radiology features and histopathological findings is made [7]. Clinically the JPOF does not display specific signs and symptoms. Some symptoms may occur while this tumor is rapidly growing, occupying intracranial space and having a mass effect on some structures with or without displacement [8]. Proptosis, displacement of the eyeball and decreasing vision are the most common signs when the anterior cranial fossa is involved. In our case report, the growth of the tumor was compromising the visual function as it was displacing the orbital content and compressing the optic nerve. CT scan and MRI can contribute to the confirmation of the diagnosis, even though there is no specific finding related to the ossifying fibroma. On CT scan it usually appears as an expansible lesion well circumcised with a typical aspect of ground glass appearance that could contain cystic component [9]. On MRI, the lesion shows intensities similar to the brain gray matter of on precontrast T1-weighted images and intermediate to low intensities on T2-weighted sequences; after gadolinium injection, there is an enhancing of the lesion [3].
The pathological specimen analysis revealing areas of high cellularity containing irregular trabeculations with major areas of the densely mineralized structure is necessary to retain the diagnosis. In our case, the histopathological examination showed tumoral proliferation well delimited from the normal neighboring tissues rich in psammomatoid ossicles set in cellular fibroblastic tissue [10]. JPOF usually tends to have a good prognosis; no malignant change or metastases have been reported [11].
The recommended treatment of JPOF is the complete removal whenever it is feasible. Therefore, when this lesion invades an important vascular and nervous structure such as the optic nerve, in this case, subtotal resection by conserving the optic nerve after decompression should be quiet enough for patient symptoms regression and better quality of life in the postoperative period. The probability of recurrence is very low, especially if the total removal is achieved [3, 12]. Many authors have described that a subtotal resection is correlated to a higher risk of recurrence; patient follow-up with repeated imaging becomes the cornerstone of the management [2, 13, 14]. Nevertheless, till now, there is no study or data that confirms a link between a recurrence and the percentage of total tumor removed. In our case, several CT scan was performed for the follow-up of the remaining tumoral fragment at 6 months, then once a year for 2 years showing that it remained sluggish.
In conclusion the skull-base location of JPOF is very rare, but it must be taken into consideration in the differential diagnoses of skull lesions. Recommended treatment is complete excision. When the removal is not complete a follow-up with a frequent radiological check-up should be considered.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
Author notes
S. El Akroud and Y.C.H. Dokponou are joint first authors.



