-
PDF
- Split View
-
Views
-
Cite
Cite
Fatemeh Hedayat, Joshua J Lauder, Panayiotis Kyzas, Leandros V Vassiliou, Internal jugular vein duplication: clinical significance for head and neck cancer ablative and reconstructive surgery, Journal of Surgical Case Reports, Volume 2021, Issue 7, July 2021, rjab300, https://doi.org/10.1093/jscr/rjab300
Close - Share Icon Share
Abstract
We present the case of a 75-year-old patient with a T2N0Mo oral cancer, who underwent surgery for cancer ablation and reconstruction. Intraoperatively, a duplicate internal jugular vein (IJV) was identified. Both segments were preserved. The veins of the free radial forearm flap that was used to reconstruct the defect were anastomosed to tributaries of the anterior IJV segment. In this rare anatomical variation, the anterior segment of IJV lies medially/anteriorly to the sternocleidomastoid muscle which poses a risk of inadvertent injury during the early steps of the neck dissection (ND). The posterior segment is at risk of injury during developing levels II–III–IV of ND. It is important to preserve the anterior IJV segment as this receives all tributaries that can be used for end-to-end anastomosis for the free flap. Preoperative contrast computed tomography scan can aid in recognition of IJV duplication and help prepare the surgeon to adjust certain operative steps.
INTRODUCTION
Neck dissection (ND) is the cornerstone of management of head and neck (H&N) cancer [1]. Brennan [2] fittingly described this procedure as walking through a jungle, using anatomical landmarks as trusted guides. One such example of a trusted guide is the internal jugular vein (IJV) that runs its ‘predictable’ course through the neck within the carotid sheath joining with the subclavian vein (SV). It is anterolaterally related to the sternocleidomastoid muscle (SCM). Deep to the SCM, it is related anterolaterally to the superior belly of the omohyoid muscle and posterior belly of the digastric muscle (DGM; [2]).
The importance of the IJV is further heightened in H&N cancer cases that require reconstruction with free tissue transfer as the IJV itself (end-to-side anastomosis) or its tributaries (end-to-end anastomosis) are the most common recipient vessels for the venous anastomosis of the free flap [3].
Anatomical variations of the IJV pose a challenge for the operating surgeon that performs the steps of the ND in a ‘standardized’ manner, assuming that the location and anatomy of the IJV is predictable and consistent. IJV duplication is an anatomical variation that occurs when the vein bifurcates into two segments, separately draining into the SV, forming a reversed-Y pattern [4]. To date, IJV duplication has been reported in 21 patients [5–7]. The important relation to the spinal accessory nerve (SAN) has been described in previous cases [8–10]; however, we report a case of a rare IJV duplication that implicates the common carotid artery between the two IJV trunks. Duplication of the IJV although previously described in the literature has not been discussed through the prism of the H&N reconstructive surgery. We aim to report the importance of this variation, specifically in the context of performing a selective ND, as well as harvesting recipient vessels for the venous anastomosis of the free flap.
CASE REPORT
A 75-year-old Caucasian gentleman was clinically staged with T2N0M0 squamous cell carcinoma (SCC) of the buccal mucosa.
The patient had a medical background of severe ischemic heart disease, hypertension, diabetes and chronic kidney disease. Due to the patient’s comorbidities preoperative staging scans included magnetic resonance imaging (MRI) of the neck and a non-contrast computed tomography (CT).
The proposed surgical treatment involved buccal SCC resection en block with rim mandibular resection and left selective ND (levels I–IV). The reconstruction would be performed with a radial forearm free flap (RFFF).
Intraoperatively, during the ND, a rudimentary only external jugular vein (EJV) was identified. Whilst developing the platysma flap, a large venous vessel was identified antero-medially to the SCM and preserved (Fig. 1). This was subsequently found to represent the anterior trunk of the duplicated IJV. Then, when developing the levels II–III–IV of the ND specimen the posterior segment of the IJV was identified and preserved. The course of IJV duplication began at level II under the posterior belly of the DGM. The bifurcation continued to level IV, beneath the omohyoid muscle. Both segments were ~9 cm in length and all the main IJV tributaries (lingual, facial and middle thyroid veins) were draining into the anterior segment (Fig. 2). The space between the two segments was occupied by the common carotid artery, its bulb and its bifurcation. The SAN was found to be running under the two IJV trunks (Fig. 3).
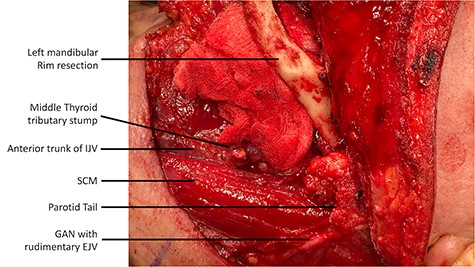
Lateral view of the left neck dissection demonstrating the anterior trunk of the duplicated IJV located antero-medially to the SCM muscle; the dissection of the greater auricular nerve and the presence of a rudimentary EJV is also known.
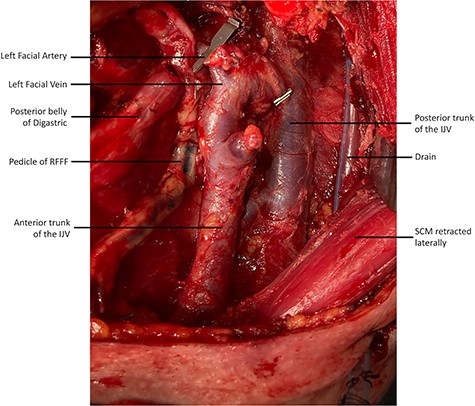
The duplicated IJV is demonstrated post-neck dissection and after the flap inset (recipient facial artery and pedicle of RFFF is shown).
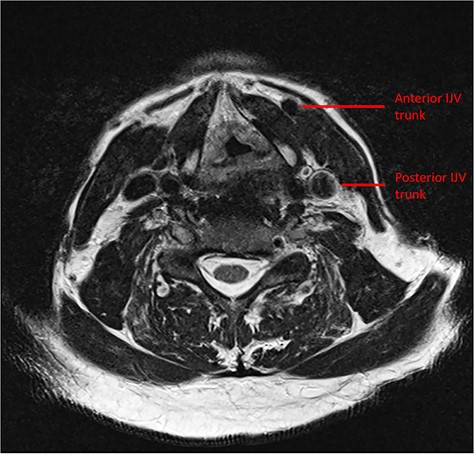
Preoperative MRI demonstrating the duplicate trunks of the left IJV.
Once the ND and the cancer ablation were completed the RFFF venous system (one vena comitans and the cephalic vein) were anastomosed end-to-end to the preserved and prepared tributaries of the anterior IJV trunk. The patient marked an uneventful postoperative course.
DISCUSSION
The strategic location of the IJV makes it an important anatomical landmark for ND [3]. Moreover, in H&N operations involving reconstruction with free flaps, the IJV and its tributaries provide the recipient veins used for microvascular anastomosis [11]. An anatomical variation may lead to inadvertent injury of this vascular structure. It is important that the surgeon is familiar with the presence of this variant, to safeguard the integrity of the vessel and use it appropriately for reconstructive purposes.
IJV duplication is a rare anatomical variation with an estimated reported prevalence of ~0.4% [5]. When it occurs, the anterior segment usually lies anterior to the SCM. Due to the antero-medial and relatively superficial location of the vessel there is a risk of inadvertent injury during the initial stages of the ND, i.e. development of the platysma flap. The vessel lies intimately beneath the superficial layer of the deep investing cervical fascia and can easily be mistaken for part of the anterior jugular drainage system. This segment must be preserved at all costs (especially in absence of an EJV) as it receives all the tributaries draining into the IJV system that are suitable for use as a recipient vein.
The posterior IJV segment is usually positioned posterior to the SCM, putting it at risk of injury when developing level IV of the ND. In level IIb, additional care should be taken when the SAN lies beneath the two IJV trunks as there is a risk of injury to the vein when dissecting through the tissue that lies superficial to the nerve.
In agreement with Wong et al. [12], we recommend the use of three-dimensional, surface rendered, CT scan for preoperative planning. This will provide the surgeon with the opportunity to clearly visualise the malformation and study its course prior to surgery. The scans could also be used in teaching settings, to help trainees appreciate this anatomical variation and learn how to overcome the challenges it presents in selective ND. In this reported case, contrast was not administered due to the patient’s comorbidities. Hence, the anatomical variation was not highlighted in the preoperative stage.
Our report highlights the clinical relevance of IJV duplication in the setting of H&N cancer ablation and reconstruction. Although this variation has previously been described, to our knowledge, this is the first article that correlates it with the aforementioned surgical implications and raises awareness to the H&N reconstructive surgeon about the potential impact on an already complex operative sequence.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.



