-
PDF
- Split View
-
Views
-
Cite
Cite
Lok Ka Cheung, Elliott Smock, Mark Pickford, Ulnar nerve compression secondary to migration of pyrocarbon implant following right wrist arthroplasty, Journal of Surgical Case Reports, Volume 2021, Issue 7, July 2021, rjab296, https://doi.org/10.1093/jscr/rjab296
Close - Share Icon Share
Abstract
A 50-year-old, right-hand dominant woman presented with a seven-month history of stiffness, pain and swelling on the ulnar side of her right wrist. She had undergone right wrist arthroplasty with a Pyrocarbon Amandys implant seven months previously for post-traumatic degenerative arthritis. She had an uneventful initial recovery until developing carpal tunnel syndrome, for which she underwent carpal tunnel release 5 months after her arthroplasty.
Examination revealed a painful and limited range of movement in the affected wrist, with weakness of the first dorsal interosseous muscle and altered sensation in the ring finger. A hard swelling was visible and palpable on the palmar-ulnar aspect of the wrist. X-rays showed that the swelling was due to the dislocated Amandys implant (which was thought to be causing compression neuropathy of the ulnar nerve). The patient underwent removal of the pyrocarbon implant (through a palmar approach) and total wrist fusion one month later, following which the wrist successfully united and all symptoms of ulnar nerve compression resolved.
Although some studies have reported migration of pyrocarbon implant following total wrist arthroplasty, to our knowledge, this is the first reported case of ulnar compression neuropathy from a migrated pyrocarbon wrist implant.
INTRODUCTION
Treating radiocarpal joint pain while preserving motion remains a challenge in wrist surgery and is yet to be satisfactorily solved. Total wrist fusion eliminates pain but comes at the cost of permanent wrist stiffness. Limited wrist fusion may be suitable in some cases but still results in a degree of stiffness, and places abnormal physiological demands on the wrist, which, over time, may result in further degenerative changes and osteoarthritis.
Total wrist arthroplasty (TWA) seeks to relieve wrist pain while preserving a functional range of motion. In practice, however, while TWA works well in the short-term, there are concerns about the longevity of TWA implants and the high rate of complications associated with them. Melamed et al. have reported that the number of TWA performed has been in decline since 2008. TWA is therefore used selectively, typically in patients with lower functional demands, in older patients and those with rheumatoid arthritis [1].
The first known TWA was performed in 1890 by Themistocles Gluck, who used an ivory ball and socket design [2]. TWA implants have undergone continuous development in an effort to ensure longevity and reduce complication rates [3, 4]. The so-called first-generation implants were silicone spacers, which had an unacceptably high complication rate; complications included implant failure, bone erosion and silicone synovitis [5].
The second-generation TWA implants were fixed to the metacarpals and distal radius with cement, but often failed due to loosening and instability [6]. Pyrocarbon is a hard, thromboresistant material with a Young’s Modulus close to bone, making it a good candidate for a bone implant. However, the long-term complications profile of Pyrocarbon Amandys wrist implants are not fully understood [7].
We report a case of ulnar nerve compression secondary to migration of a Pyrocarbon Amandys implant. The patient provided informed consent to publish this case report, clinical photographs and radiographs.
CASE REPORT
A 50-year-old, right-hand-dominant woman, presented with a history of stiffness and pain affecting her right wrist, associated with a history of increasing swelling on its palmar aspect. She had been treated for post-traumatic arthritis of the same wrist 7 months earlier by arthroplasty with a Pyrocarbon Amandys implant; she also reported gradual onset of tingling sensations in her ring finger. She had an initial uneventful recovery but developed clinical symptoms of carpal tunnel syndrome 2 months later, with paresthesia in the right thumb and index finger radiating to the forearm, which was worse at night. A diagnosis of carpal tunnel syndrome was confirmed by nerve conduction studies. Post-operative radiograph at this time showed the pyrocarbon implant in an adequate position (Fig. 1).

The patient underwent carpal tunnel release at 5 months post-operatively; the delay in treatment was deliberate, in order to allow conservative healing of a fractured surgical neck and greater tuberosity of the right humerus, which had occurred at 3 months post-operatively due to a mechanical fall from standing height (note—the ipsilateral wrist was not injured by the fall).
On examination, a hard swelling was present on the palmar-ulnar aspect of the wrist. Range of motion in the wrist was extremely limited and painful; there was also significant weakness of the first dorsal interosseous muscle (without wasting), but full power in the abductor digit quinti. Static two-point discrimination was within normal limits in the tips of all digits.
Radiographs demonstrated that the Pyrocarbon implant was palmarly displaced and rotated 90 degrees; it had migrated into the carpal tunnel/ distal forearm (Fig. 2). The clinical diagnosis was compression of the ulnar due to the migration of implant. Surgery was carried out 1 month later during which the Pyrocarbon Amandys wrist implant was removed through a volar approach (Fig. 3) and total wrist fusion was performed using a straight Arbeitsgemeinschaft für Osteosynthesefragen (AO) wrist fusion plate (Fig. 4). The surgery successfully relieved all wrist pain and was accompanied by prompt resolution of symptoms of ulnar nerve compression; she was discharged from follow-up approximately 3 months after surgery.

X-rays of the right hand showed palmar displacement of the pyrocarbon implant.
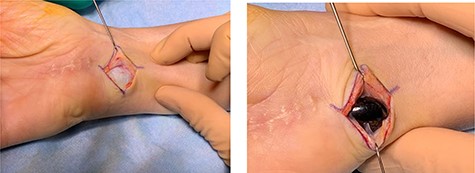
Intra-operative clinical photographs of the migrated pyrocarbon implant.
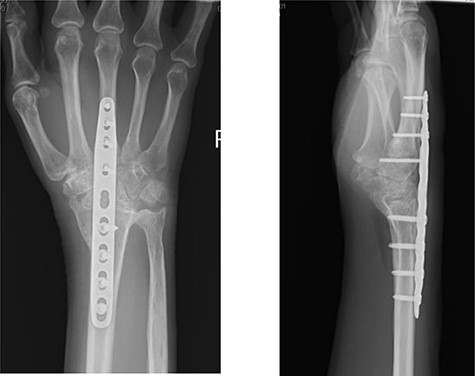
Post-operative radiographs following removal of pyrocarbon implant and total wrist fusion.
DISCUSSION
The Amandys wrist implant is inserted using a dorsal approach to the wrist between the third and fourth extensor compartments. Radial styloidectomy is routinely performed to allow the implant to be accommodated with the wrist in a neutral (flexion-extension) position; there is a risk of detachment of important palmar extrinsic ligaments of the wrist if excess bone is removed. The proximal portion of the scaphoid, the entire lunate and a small section of capitate are removed. The correct implant size is fitted, using fluoroscopy to assess implant/ wrist stability during extremes of movement [7].
The volar extrinsic ligaments of the wrist may be damaged during the removal of lunate, which could predispose to volar migration of the implant into the carpal tunnel. Incomplete resection of the lunate is therefore recommended to avoid such an outcome [7].
In the case presented, the Pyrocarbon implant was dislocated palmarly and was 90 degrees rotated causing ulnar nerve compression; there was a history of a mechanical fall 3 months post-operatively. Although trauma may have played a role in the mechanical displacement of the Amandys implant in this case, it is possible that the volar extrinsic ligaments may have been compromised during the insertion of the implant predisposing to volar migration of the implant.
In 2012, a prospective study showed volar displacement of a pyrocarbon wrist implant within 1 month when allowed to mobilize gently immediately after the operation [7].
Currently, no long-term outcomes for pyrocarbon wrist arthroplasty are available. However, a cohort study looking at trapeziometacarpal joint replacement with pyrocarbon interposition showed a prolonged operative time and risk of implant displacement compared with simple trapeziectomy [8]. Furthermore, a 10-year follow-up study of 12 Pyrocarbon implants used for proximal interphalangeal joint replacement showed a high migration rate, this was attributed to problematic implant fixation [9].
Early unrestricted mobilization following operation, as well as volar extrinsic ligament damage may contribute to migration of Pyrocarbon Amandys implants; a fall onto the operated limb, as experienced in the case presented, might also contribute to implant displacement. Long-term outcome studies are needed to fully understand the risks associated with the use of Pyrocarbon Amandys implants.



