-
PDF
- Split View
-
Views
-
Cite
Cite
Khalid Saad Almousa, Mohammed Nabeel Refka, Late-onset capsular bag distention syndrome resistant to laser treatment: a case report, Journal of Surgical Case Reports, Volume 2021, Issue 7, July 2021, rjab278, https://doi.org/10.1093/jscr/rjab278
Close - Share Icon Share
Abstract
Capsular bag distention syndrome (CBDS) or capsular block syndrome is a rare complication of cataract surgery. Neodymium-doped yttrium aluminum garnet (Nd:YAG) laser usually is effective treatment for CBDS. Rarely, surgical intervention is required in resistant cases (as in our case). Herein, we present the case of a 58-year-old male who presented to us with this condition.
INTRODUCTION
Capsular bag distention syndrome (CBDS) or capsular block syndrome is characterized by the entrapment of fluid between the intraocular lens (IOL) and the posterior capsule. The estimated incidence of CBDS is 0.73% [1]. It has been classified based on the onset time by Miyake et al. [2] as intra-operative (after hydrodissection), early post-operative (1–15 days after the surgery) and late post-operative (lacteocrumenasia).
Clinically, the patients can be asymptomatic or present with decreased visual acuity in the affected eye because of the entrapped milky fluid and/or myopic shift [3]. The preferred treatment option is Neodymium-doped yttrium aluminum garnet (Nd:YAG) laser posterior capsulotomy for the majority of symptomatic CBDS cases. However, in some cases (as in our case), surgical intervention is needed to evacuate the turbid fluid, either by anterior or posterior approaches.
CASE DESCRIPTION
A 58-year-old male with a history of diabetes mellitus and hypertension presented at our clinic complaining of gradual painless decreased vision in his left eye over the last year. He underwent cataract surgery for both eyes outside our facility 2 years before the presentation.
There was no history of pain, photophobia or floaters. His best corrected visual acuity during the first visit was 20/28 in the right eye and 20/2000 (ability to count fingers at 4 feet) in the left eye. Intra-ocular pressure was 18 mmHg in the right eye and 20 mmHg in the left eye. Subjective refraction did not yield better vision in the left (affected) eye.
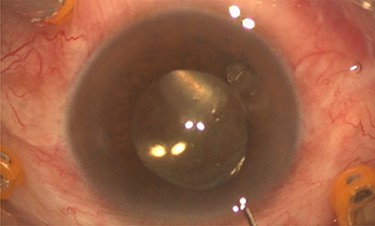
On examination, both eyes showed a quiet conjunctiva with clear corneas and quiet pseudophakia. Anterior chamber was deep and equal in both eyes. Left eye showed dense turbid fluid behind the IOL, with multiple pitting on the IOL, indicating a previous trial of Nd:YAG capsulotomy (Fig. 1). Posterior capsule could not be visualized by the slit lamp. Right eye showed a clear capsular bag with a good view of the fundus. Fundus exam showed mild non-proliferative diabetic retinopathy and dry macula in the right eye and no view of the fundus in the left eye.

Pre-operative slit lamp photo showed turbid fluid behind the IOL, and the IOL pitting indicates a previous trial of YAG capsulotomy.
Ultrasound biomicroscopy (UBM) showed dense turbid fluid behind the IOL with varied echogenicity, a severely distended capsular bag, and a thick irregular posterior capsule (Fig. 2). Based on the previous findings, a diagnosis of late onset CBDS was made.
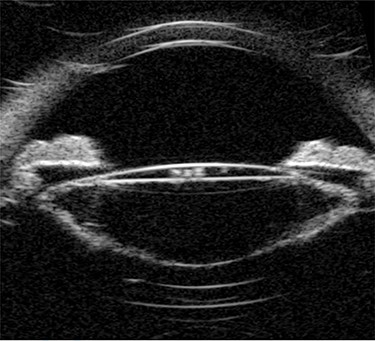
Pre-operative UBM shows a markedly distended capsular bag and thickened posterior capsule.
Due to the poor visibility of the posterior capsule and the overblown capsular bag, surgical intervention using a posterior approach was selected to facilitate surgical capsulotomy without disturbing the position of the IOL and to have better access to aspirate the trapped fluid.
Pars plana vitrectomy and posterior capsulotomy were done. After placing three 23-gauge trocars, a corneal paracentesis was made. After IOL tapping, the entrapped turbid fluid escaped to the anterior chamber (Fig. 3). Anterior vitrectomy and posterior capsulotomy were done using a 23-gauge vitrector (Fig. 4).
Intra-operative photo showed egression of turbid fluid to the anterior chamber.
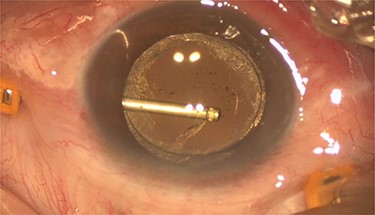
Intra-operative photo showed the posterior capsulotomy using 23G vitrector.
During the first post-operative visit, the patient exhibited better vision with a visual acuity of 20/125. The patient reached 20/60 vision after 1 month post-operatively.
DISCUSSION
Several risk factors for CBDS have been reported in the literature. Residual cortical material is a well-known risk factor, resulting in a milky fluid due to the secretion of alpha crystalline proteins [4]. Other factors include retainment of the ophthalmic viscoelastic device possibly by an osmotic gradient mechanism [2, 3, 5], longer axial length [1] and smaller continuous curvilinear capsulorhexis or larger IOL design because of which the IOL and anterior capsule overlap area is larger, resulting in, the occlusion of the intra-capsular fluid egression pathway [6].
Various diagnostic tools have been used to diagnose CBDS, including slit-lamp biomicroscopy, UBM, anterior segment optical coherence tomography and Scheimpflug-based photography [7]. Propionibacterium acnes (P. acnes) has been reported in some studies, following the diagnostic aspiration of intracapsular fluid for CSBD [8, 9]. Thus, P. acnes might play a role in the pathophysiology of the disease, keeping in mind that P. acnes endophthalmitis after Nd:YAG capsulotomy has been reported [10, 11]. Therefore, careful assessment to rule out chronic endophthalmitis is important since the Nd:YAG capsulotomy might induce or worsen endophthalmitis.
Pars plana vitrectomy and posterior capsulotomy for CBDS have not been adequately studied. As in our case, surgical intervention by pars plana vitrectomy and posterior capsulotomy has several advantages over other approaches, including a lower risk of P. acne endophthalmitis or inflammation, which might be aggravated by Nd:YAG or anterior approach capsulotomy [4], and the prevention of a possible rise in the intraocular pressure caused by collagen in the milky fluid that might clog the trabecular meshwork [12].
However, apart from the known possible complications of pars plana vitrectomy, it is also considered to be more invasive and costly [4].
Bhattacharjee et al. [13] reported 11 cases with delayed onset CBDS treated surgically, and all the patients ended up with 20/20 vision, indicating a good prognosis for this syndrome after proper management.
CONFLICT OF INTEREST STATEMENT
None declared.



