-
PDF
- Split View
-
Views
-
Cite
Cite
Theresa Kastiunig, Rosita Sortino, Larissa Clea Vines, Luca Benigno, Intra-abdominal foreign body as unexpected discovery mimicking suspicious malignancy, Journal of Surgical Case Reports, Volume 2021, Issue 6, June 2021, rjab248, https://doi.org/10.1093/jscr/rjab248
Close - Share Icon Share
Abstract
Although rare, postoperatively retained foreign bodies in the abdominal cavity still represent a serious issue for the surgical team as for the patients. Its clinical manifestation is often unspecific and the cases are therefore only irregularly registered.
There are several known factors that increase the risk of retention of a foreign body, for example emergency surgeries, unplanned changes in procedure or a high body mass index.
In this article, we would like to report the case of a male patient with a foreign body in the right lower quadrant after open appendectomy mimicking a tumor.
INTRODUCTION
Retained foreign bodies (RFB) may cause serious complications or remain undetected for years. Possible symptoms range from discomfort, pain, nausea and vomiting to peritonitis [1]. Potentially arising complications include abscesses, fistulas and intestinal obstruction [2].
Numerous safety checks like counting surgical instruments and sponges before ending the procedure were introduced in the last years to avoid these major complications. We report a case of a suspected tumor in the right mesocolon >15 years after open appendectomy.
CASE REPORT
A 63-year-old male was hospitalized at our department with nausea, vomiting and constipation. The only prior surgery was an open appendectomy 15 years earlier.
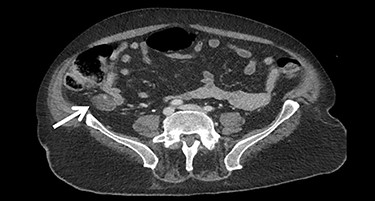
A gastroscopy showed a gastroparesis but no other pathologies. The next diagnostic step was a computed tomography (CT) scan, which showed a suspicious extraluminal mass in the right abdomen close to the terminal ileum (Fig. 1).
Tumor markers were negative, except for insulin and C-peptide. Urinary catecholamines were slightly increased.
At an interdisciplinary tumor board primary resection was recommended because a neuroendocrine or gastrointestinal stromal tumor could not be excluded.
A laparotomy was performed showing chronic gastroparesis and adhesions. In the right lower quadrant we found a 3 × 5 cm compact foreign body in the right mesocolon, which was carefully removed (Fig. 2). Upon closer examination a crumpled surgical glove was revealed (Figs 3 and 4). The planned right hemicolectomy could therefore be prevented. The postoperative course was uneventful and the patient was discharged in good general condition on the fifth postoperative day.



How an almost entire glove ended up in the abdominal cavity remains unclear. Whereas digits of gloves have been known to be used as a low-cost and easily available replacement for drains, entire gloves are usually not left behind on purpose.
DISCUSSION
RFB may cause early complications or various symptoms after months or even years. Sometimes they remain altogether asymptomatic. The clinical manifestation ranges from no symptoms at all to pain, sepsis, abscess, nonhealing wounds, fistulas and intestinal obstruction [1, 3, 4].
The incidence of RFB is ranging between 1 in 1.000 and 1 in 1.500 abdominal interventions with a continuous decrease between the 1980s and nowadays. The numbers are somewhat unreliable as many cases remain asymptomatic and there is a certain reluctance of hospitals to disclose sensitive data on adverse events. However, it is estimated that one or two RFB incidents occur during the course of a surgeon’s professional life [5].
The incidence might be even higher during emergency surgeries [6]. A surgical sponge is the most commonly reported retained item following surgery, whereas reports of retained needles and instruments are extremely rare [3]. There are cases of retained appendices epiploicae after surgery resembling a ‘boiled egg’ [7].
A multivariate analysis showed that the incidence is associated with main risk factors like high body mass index in patients, emergency procedures and unplanned changes in the procedures performed. Other risk factors include changes of the operating team during a procedure, a significant loss of blood (>500 ml), abstaining from counting instruments following a procedure and excessive fatigue of the medical staff [5, 8, 9].
The gold standard for further diagnostics when suspecting a RFB is a CT. In case of RFB the CT scan can demonstrate a well-defined mass of mixed density with a thick peripherally rim enhancement, often calcified with a possible abscess formation. A ‘spongiform pattern’ is typical. The use of surgical sponges with radiopaque markers is highly recommended. On plain radiograph a curved or banded radiopaque line might be observed. Magnetic resonance imaging and other relevant radiological techniques may also be used depending on the clinical situation [1, 2].
Treatment options include minimally invasive techniques (endoscopy or laparoscopy) or open surgery. Endoscopy can be used for removal of the RFB if it has already migrated into hollow organs such as the stomach and the large intestine. A diagnostic laparoscopy might help securing the correct diagnosis but does sometimes not prove useful in retrieving the RFB as they are usually large, impacted and have caused multiple adhesions [1].
In conclusion, RFB are an actual problem in the postoperative complication rate. The key point is minimizing errors by reducing distractions, using a consistent counting method and avoiding interruptions while counting [2]. If not all sponges and instruments are accounted for, an exploration or an on-table X-ray is to be performed. It has been shown that the count is reported as ‘correct’ in 88% of cases of patients with RFB [8].
The best way to prevent RFB is a good communication between surgeons and nurses as well as a correct count of instruments and sponges [10]. However even today, a correct sponge count unfortunately does not fully exclude a retained sponge. So if in doubt the operative field should be closely inspected once again or an X-ray should be taken [6].
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



