-
PDF
- Split View
-
Views
-
Cite
Cite
Jamil Suleiman, Alex Mremi, Murad Tarmohamed, Adnan Sadiq, Jay Lodhia, Concealed gallbladder perforation: a rare case report, Journal of Surgical Case Reports, Volume 2021, Issue 6, June 2021, rjab245, https://doi.org/10.1093/jscr/rjab245
Close - Share Icon Share
Abstract
Acute acalculous cholecystitis remains an elusive clinical diagnosis possibly due to complex clinical setting in which this entity develops, lack of large prospective controlled trials that evaluate various diagnostic modalities, thus dependence on a small database for clinical decision making. Concealed gallbladder perforation is rare. Herein, we report an 82-year-old female who presented with a right upper quadrant pain and features of local peritonitis. Abdominal ultrasound was suggestive of cholecystitis while computed tomography (CT) scan reported a perforated gallbladder with pericholecystic fluid collection. The patient underwent successful cholecystectomy; and intra-operatively, similar findings as those reported on imaging were seen. Unfortunately, she succumbed shortly post-operatively due to pulmonary embolism. Our report highlights the importance CT scan in patients with vague abdominal symptoms followed by sudden resolution. It also reminds the importance of considering the diagnosis of concealed gallbladder perforation as a differential in patients with peritonitis, as it may be missed by routine radiological investigations.
BACKGROUND
Gallbladder perforation causes peritonitis hence is a surgical emergency [1]. Inflammation of the gallbladder usually causes perforation, which can be due to cholecystitis or malignancy [1–2]. A standard management approach involves a fine balance between the diagnostic and interventional services for these patients. This case highlights the importance of computed tomography (CT) scan in patients who present with vague abdominal symptoms followed by sudden resolution and negative signs.
CASE PRESENTATION
An 82-year-old female, with a history of hypertension for the past 10 years; and on amlodipine, presented to the emergency department (ED) complaining of sharp right upper quadrant pain for 1 day. The pain was of sudden onset, and progressively worsened, not associated with nausea or vomiting, or any changes in bowel habits. Her vital signs were: blood pressure of 144/89 mmHg, pulse rate of 66 beats/min, body temperature of 37 degrees Celsius; respiratory rate of 19 breaths/min and was saturating at 99% in room air. During physical examination, she was in agonizing pain, afebrile, not pale and not icteric. She had severe tenderness on the right hypochondriac region extending to the epigastric region, with Murphy’s sign positive and positive rebound tenderness indicating local peritonitis. At the ED, the patient was given tramadol to control the pain, and intravenous antibiotics were initiated. Chest X-ray, electrocardiography and other parameters were within normal range. Blood workup was done and showed a raised alanine aminotransferase of 50.30 U/L, (2.00–41.00). An abdominal ultrasound was performed, which showed a shrunken gallbladder with increased wall thickness-5 mm in size, and an impression of cholecystitis was made. A few hours post admission, the rebound tenderness was lost and hence an abdominal CT scan was ordered, for a confirmatory diagnosis. The abdominal CT scan reported diffuse thickening of the gallbladder with pericholecystic fluid collection. Perforation of the gallbladder was noted, with contained fluid collection around the transverse colon (hepatic flexure). No gallbladder calculus or mass was seen. Features were suggestive of perforated cholecystitis (Fig. 1). The patient was planned for an open cholecystectomy; the abdomen was then entered via a right Kocher’s incision. The gallbladder was identified and a concealed perforation was seen at the upper body, pulling the epiploic appendages of the transverse colon (Fig. 2). The appendages were released and a retrograde cholecystectomy was done. Hemostasis was achieved and the abdomen was closed in layers. Post-operative antibiotics and analgesics were given.
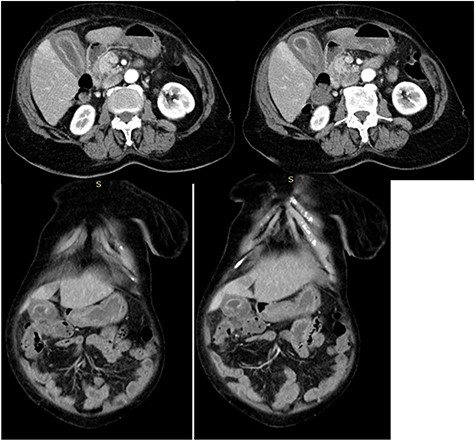
CT axial and coronal images of the abdomen showing diffuse thickening of the gall bladder with pericholecystic fluid collection; gallbladder perforation and fluid collection around the transverse colon (hepatic flexure) suggestive of contained perforated acalculuscholecytitis.

Concealed perforation at the fundus (arrow) pulling the epiploic appendages of the transverse colon.
In the ward, 6 hours post-operatively, the patient had stable hemodynamic measurements but suddenly she started experiencing an onset of difficulty in breathing. Upon examination, she had a respiratory rate of 27 breaths/min, de-saturating at 75% in room air. She increasingly became hypotensive over time with a blood pressure of 75/50 mmHg, and had a tachycardia of 110 beats/min. A presumptive diagnosis of pulmonary embolism was made with a modified well’s score of 3. An immediate single dose of heparin was given, together with oxygen supplementation via a non-rebreather face mask and intravenous fluids. A few minutes later, the patient was found unresponsive with no signs of life despite resuscitative efforts. Clinical post mortem was requested but unfortunately because of tradition and cultural beliefs, the authorization for the procedure was declined. Histopathology results of the gallbladder confirmed acalculus cholecystitis (Fig. 3).

Photomicroscopy of gallbladder tissue demonstrating chronic cholecystitis characterized by wall thickening, edema and necrotizing inflammation secondary to perforation; H&E staining ×20 original magnification (A); and ×40 original magnification (B).
DISCUSSION
Gallbladder perforation is a rare pathology but a known complication of cholecystitis with an incidence of 2–11% and a mortality rate of 0.8–11% [3]. One of the complications of acute cholecystitis is a pericholecystic abscess with a prevalence of 2.1–19.5% reported in different case series [4]. Like in our case, this is usually seen not only in the elderly group, but also in those with immunosuppression, co-morbidities like diabetes mellitus, atherosclerosis or organ failure. A recent article by Bruni et al. [5] presented that SARS-CoV-2 can cause cholecystitis hence lead to perforation. Our patient, however, was not screened for COVID-19 because during admission she did not meet the criteria set by Centres for Disease Control and Prevention for COVID-19 testing.
The fundus is the most common site of perforation, as also seen in the index case, accounting for 60% [3]. There are four types of perforation. Type-1 include acute perforation with generalized peritonitis, type-2, subacute with localized pericholecystic abscess, type-3 is chronic perforation with cholecysto-enteric fistula and type-4, chronic perforation with cholecysto-biliary fistula [6].
Certain cases have been reported of asymptomatic gallbladder perforations in literature [1]. Like in the index case, this can happen in those whose perforation is sealed by the omentum and/or bowel or in those who are diabetic due to the related neuropathy and ischemic changes. Similarly to our case, Faraji et al. also presented a case where the patient had resolved abdominal signs but the CT scan revealed a perforated gallbladder while the ultrasound was negative [1]. This emphasizes that surgeons need to have a high index of suspicion whenever symptoms are either vague or resolved, and as ultrasonography can miss the pathology, a CT scan should be opted for such scenarios [7]. Alshargi et al. [8] concluded in their report that CT scans are the most effective technique for challenging gallbladder conditions.
In conclusion, perforation of the gallbladder is a natural disease process resulting from the sequelae of inflammation with significant morbidity and mortality. Thus, early management is needed; and surgeons should have a higher index of suspicion and a low threshold for higher radiological modalities like CT scan for patients who present with indistinct abdominal symptoms.
INFORMED CONSENT
Written informed consent was obtained from the patient for publication for this case report; additionally, accompanying images have been censored to ensure that the patient cannot be identified. A copy of the consent is available on record.
ACKNOWLEDGEMENTS
The authors would like to thank the patient for permission to share her medical information to be used for educational purposes and publication.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
AUTHORS’ CONTRIBUTIONS
J.S. and J.L. conceptualized and drafted the initial manuscript. M.T. was the lead surgeon. A.M. performed histopathological investigation and was responsible for preparing the final manuscript version. A.S. reviewed and reported the radiology scans. All authors have read and approved the final script.



