-
PDF
- Split View
-
Views
-
Cite
Cite
G Calugi, W Dorigo, A Capone, D Esposito, E Giacomelli, C Pratesi, Acute limb ischemia due to ONYX 34 migration during embolization of a traumatic pseudoaneurysm of the superficial femoral artery, Journal of Surgical Case Reports, Volume 2021, Issue 6, June 2021, rjab231, https://doi.org/10.1093/jscr/rjab231
Close - Share Icon Share
Abstract
Pseudo-aneurysms of the arteries of the lower limbs are a possible complication of leg trauma. Complications include rupture, infection, pain and distal embolization. This is a case of a 24-year-old man hospitalized after a car accident, in which we discovered a 1-cm large pseudo-aneurysm of the right superficial femoral artery. The pseudo-aneurysm in first place was treated by the interventional-radiologist for an endovascular repair by embolization with ONYX 34, but during the procedure the copolymer embolized in the arterial axe with complete obstruction of blood-flow in the lower limb. An urgent open surgical revascularization was then attempted by our team with the result of complete patency of the femoro-popliteal axis and of the tibial vessels. Embolization with ONYX is an effective and safe method, but it is susceptible to this type of complication for larger pseudo-aneurysms, where it is required an introduction of a larger quantity of polymer.
INTRODUCTION
Pseudo-aneurysms of the arteries of the lower limbs are a possible complication of leg trauma. Complications include rupture, infection, pain and distal embolization [1].
The possible treatments are surgical repair, ultrasound guided compression, endovascular techniques and injection of pro-thrombotic agents. Among them, ethylene-vinyl alcohol copolymer (ONYX) is assuming an important position [2]. Few data do exist concerning complications of ONYX in such conditions.
We describe a case where there has been migration of this polymer during embolization of a post-traumatic pseudo-aneurysm of the superficial femoral artery (SFA).
CASE REPORT
A 24-year-old man was hospitalized after a car accident. He was found unconscious with a GCS (Glasgow Coma Scale) of 5.
During hospitalization, the patient underwent many orthopedic surgeries for various fractures of the right lower limb, and a centimetric pseudo-aneurysm of the right SFA (Fig. 1), was found at a routine duplex ultrasound of the lower limbs, originating from a small collateral branch of SFA at the distal third of the thigh.
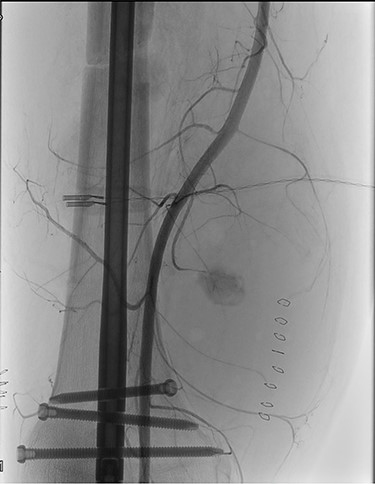
Preoperative angiography showing the pseudo-aneurysm of the right SFA, originating from a small collateral branch of SFA at the distal third of the thigh.
The consultant interventional-radiologist indicated the need for an endovascular repair of the lesion. Through percutaneous puncture of the left common femoral artery, selective catheterization of the right SFA was performed, and embolization of the pseudoaneurysm and the tract of the artery downstream of it, was completed with ONYX 34.
At the retraction of the micro-catheter a reflux of embolization agent occurred in the femoral superficial artery to then migrate in the distal vessels.
An emergency vascular surgery consultation was required. Upon our arrival, the foot was hypothermic and pale, with pain and paraesthesia. At the angiography, near occlusion of the SFA at its middle third was found, with concomitant occlusion of the popliteal artery and of the leg arteries (Fig. 2).
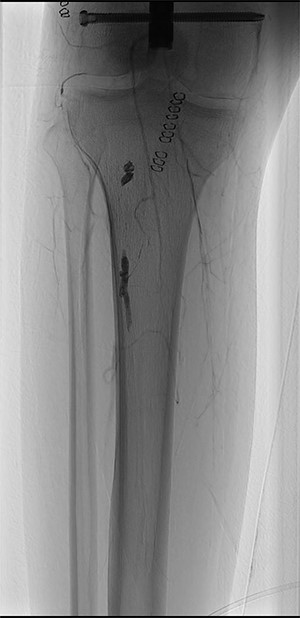
ONYX 34 residuals in the distal popliteal artery and in the tibioperoneal trunk obstructing blood-flow in the right lower limb.
The CW-Doppler examination showed absence of distal arterial flow and an urgent surgical revascularization was unavoidable.
An incision of the superior third of the leg was made with isolation of the popliteal artery and its trifurcation. An incision at the distal third of the thigh with isolation of the SFA was then performed. At arterial clamping 1500 international-units of sodium heparin were administered intravenously.
A consistent hematoma was drained and the afferent artery to the pseudo-aneurysm was sutured. Then an intraoperative angiography was made to localize ONYX residuals.
A transverse incision of the distal SFA was then performed with removal of the ONYX residual and primary closure of the arteriotomy. Via a longitudinal arteriotomy extended from the distal third of the popliteal artery to the tibio-peroneal trunk up to its bifurcation, the other ONYX residues were then removed. Due to the concomitant thrombosis of the tibial vessels, thrombectomy under fluoroscopic guidance of the anterior tibial, posterior tibial and peroneal arteries was carried out. A polyurethane patch was then applied to close the arteriotomy, due the unavailability of adequate saphenous vein segments.
Completion angiography demonstrated the patency of the femoro-popliteal axis and of the tibial vessels (Fig. 3). Anterior and posterior fasciotomy of the leg was performed. At the end of the procedure a CW-Doppler was made showing triphasic-flow in the anterior and posterior tibial artery.

Completion angiography demonstrating patency of the popliteal artery, anterior tibial artery, posterior tibial artery and peroneal artery.
In the following days the right lower limb appeared warm and perfused to the ankle, with thermic difference with the foot that appeared cold, without motor and sensory deficits.
This situation improved with demonstration after 10 days, of a warm and perfuse lower limb with triphasic-flow on tibial vessels.
At the Doppler examinations after 2 and 12 months, triphasic-flow of the entire vascular artery axe of the lower right limb was detected (Fig. 4).
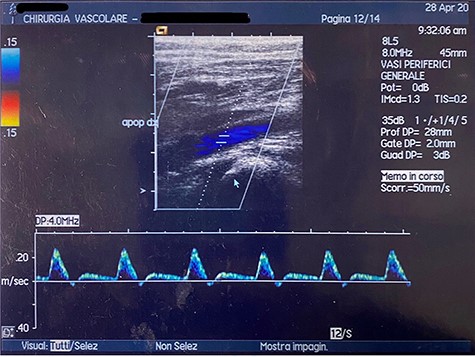
Duplex ultrasound made after 2 months, showing triphasic flow of the right popliteal artery.
DISCUSSION
ONYX is a biocompatible liquid embolic agent that when it comes in contact with blood, it causes in situ precipitation and solidification of the polymer, forming a solid-spongy embolus not adherent to the vascular lumen [2]. ONYX is not a glue, but an occlusive mechanical agent, without the risk of a potential catheter gluing [2]. Its advantages are easy handling, progressive solidification and weak inflammatory effect on the endothelium [3]. The main risk is embolization in distal vessels, which has been however rarely described.
Ierardi et al. [4] reported a case of migration of ONYX in the urinary tract after embolization of the renal artery, whereas Urbano et al. [5] described a case of selective embolization in massive bleedings of the gastrointestinal-tract followed by migration of ONYX in the distal arterial bed and risk of bowel ischemia.
In literature there are no reports dealing with the migration of ONYX in the arteries of the lower limb. We reported a case of leg ischemia due to ONYX migration following an attempt of endovascular treatment of a post-traumatic femoral pseudoaneurysm.
This patient had a small pseudoaneurysm, with a neck around 3 mm, in a deep position, difficult to treat with compression, making it suitable for an endovascular approach.
We suppose that distal embolization is associated with the use of a quantity of ONYX higher than necessary, that created a pressurization of the pseudo-aneurysmatic sac and once the introducer was removed the copolymer migrated with consequent complete obstruction of the three leg vessels.
Luckily, the characteristics of the non-adherence of the polymer to the vessels wall made it possible for it to be removed with complete recanalization of the leg vessels.
This case reports that even if rare, complications of ONYX in the arterial axe are severe.
Embolization with ONYX is an effective and safe method, but it is susceptible to this type of complication for larger pseudo-aneurysms, where a larger quantity of polymer is required.
Other types of approach could have been: (i) ultrasound-guided percutaneous thrombin injection, directly in the pseudo-aneurysm creating thrombosis of the sac; (ii) balloon assisted thrombin injection, where a balloon catheter is used to prevent possible spillage of thrombin and (iii) covered stent or coil embolization that involves the filling of the pseudo-aneurysm with coils to occlude blood-flow [1].
In our opinion, in this patient, an open surgical approach would have been more adequate and resolutive; Even considering that open surgery is burdened by greater invasiveness, risk of wound dehiscence and higher risk of infection.
FUNDING
The study is unfunded.
CONFLICT OF INTEREST STATEMENT
All the authors have no conflict of interest to disclose.



