-
PDF
- Split View
-
Views
-
Cite
Cite
Rommel Ojeda, Gabriel A Molina, Galo E Jiménez, Hernán González, Johanna C Pinto, Andres Jiménez, Flor M Leon, Sclerosing angiomatoid nodular transformation (SANT) of the spleen: a rare cause of acute abdomen, Journal of Surgical Case Reports, Volume 2021, Issue 4, April 2021, rjab126, https://doi.org/10.1093/jscr/rjab126
Close - Share Icon Share
Abstract
Sclerosing angiomatoid nodular transformation (SANT) of the spleen is an extremely rare benign lesion. It originates from the spleen's red pulp; however, its pathogenesis is not clearly defined. These tumors are usually asymptomatic or cause nonspecific abdominal symptoms. Most SANTs are found incidentally on radiographic examination or during surgery for an unrelated condition. The differential diagnosis from other splenic tumors or malignant lesions can be challenging due to the risk for a possible malignancy of the suspicious lesion. As more SANTs are being discovered and treated, they should always be considered in the differential.
We present the case of an otherwise healthy 30-year-old female; she presented with abdominal pain and a mass in her spleen. Surgery was performed, and an SANT was discovered. The patient underwent full recovery, and on follow-up is doing well.
INTRODUCTION
Sclerosing angiomatoid nodular transformation (SANT) is a rare benign disease of the spleen [1, 2]. Clinical symptoms are nonspecific, and a suspicious splenic lesion is often suspected, leading to splenectomy [2, 3]. Diagnosis is usually made histologically after complete resection. We report a 30-year-old female. She presented to the emergency room with acute abdomen. A splenic mass was identified, and surgery was completed. SANT of the spleen was discovered; on follow-ups, the patient is doing well.
CASE REPORT
Patient is a 30-year-old female without past medical history. She had a 1-year history of mild abdominal pain in her upper left abdomen; at first, the pain was mild; nonetheless, the pain became much more severe throughout the year and was accompanied by nausea. Thus, she presented to the emergency room. On clinical examination, abdominal pain and tenderness along with a solid mass with severe pain on touch were discovered in her upper abdomen. No fever, vomiting, blood in the stool, or other symptoms were found. Due to this, a computed tomography (CT) revealed an enlarged spleen. It measured 15 × 10 × 5.5 cm, and within the spleen, a 5.4 × 5.1 cm mass and another 5.3 × 2.3 cm mass is seen (Fig. 1A and B). Laboratory exams revealed leukocytosis with neutrophilia and an elevated C-reactive protein.
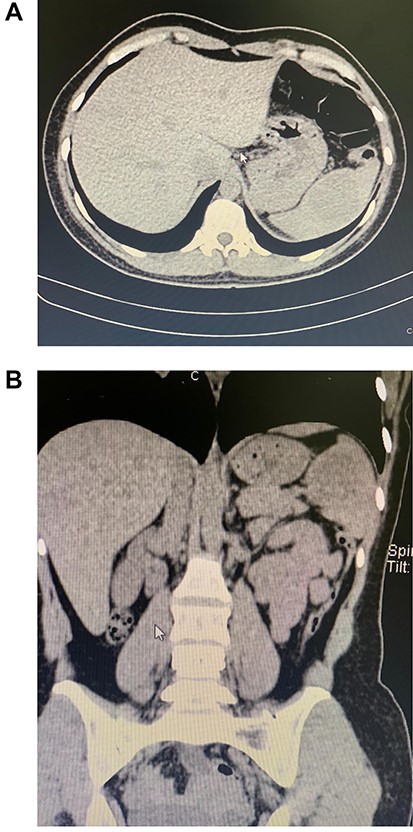
(A) CT, a mass is seen in the spleen. (B) CT, the enlarged spleen with the mass in the upper pole.
With these findings, surgery was needed, and a laparoscopic approach was decided. The enlarged spleen had multiple hemorrhagic foci in its capsule. The larger mass was located mostly on its upper lobe. No other masses, free liquid or lymph nodes were found. Due to this, a laparoscopic splenectomy was completed. Pathology revealed a 15 × 10 × 5.5 cm spleen with a 5.4 × 5.1 cm mass in its upper lobe and a 5.3 × 2.3 mass on its lower lobe; the masses had a yellowish color and had multiple nodules (Fig. 2A and B). Multiple angiomatoid nodules were embedded in a fibrosclerotic stroma; many regions showed increased vascularity, and strong positivity for CD34 was detected on microscopic evaluation (Fig. 3A and B). SANT was the final diagnosis.
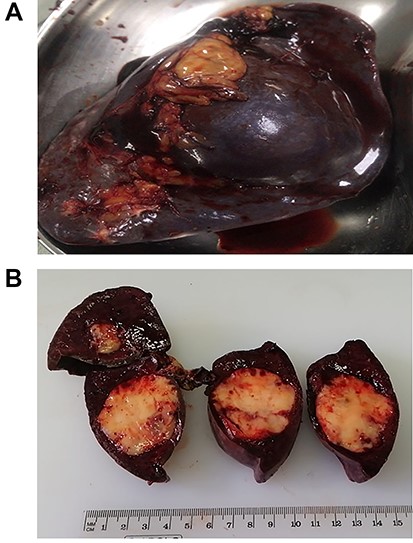
(A) Spleen completely resected. (B) White SANT masses within the spleen.
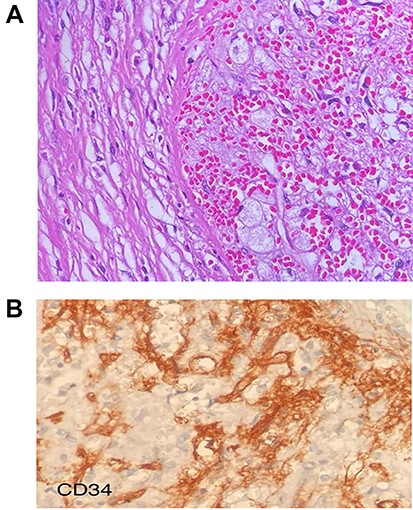
(A) Multiple angiomatoid nodules embedded in a fibrosclerotic stroma. (B) CD34 were detected on microscopic evaluation on the stroma.
She was discharged on her second postoperative day after a full diet was initiated. The patient was checked at regular intervals after surgery. Immunization was given, and no sign of recurrence was detected until the first year after surgery.
DISCUSSION
Tumors of the spleen are rare [1]. Their classification is varied, but they are usually classified into two main categories: nonlymphoid and lymphoid [1, 2]. The most common primary malignancies of the spleen are lymphoma and angiosarcoma [1]. Metastasis to the spleen is extremely rare (2.3–7.1%) and usually found during autopsies from cutaneous malignant melanoma and breast cancer [1, 2]. The majority of nonlymphoid primary tumors of the spleen are of vascular nature and are usually cavernous hemangiomas [2, 3]. Nonetheless, in 2004, Martel et al. described a rare primary benign tumor-like lesion of the spleen with its own pathological features and immunohistochemical profile [1, 2]. The name SANT of the spleen appeared [2]. Although it was first reported in 1978 by Silverman and LiVolski and defined as a special kind of hamartoma, Martel et al. were the ones that defined its characteristics [2, 3].
SANT can be distinguished from other tumors as the angiomatoid nodules are composed of splenic red pulp elements, and its borders are microscopically defined [1, 4]. However, its etiology is still under study. It is believed that SANT tends to affect middle-aged women as a benign hyperplastic neoplastic disease, not a neoplasm, but a reactive vascular lesion that can be cured by surgery [1, 5]. Our patient was a young female without any comorbidity. SANT are sporadic tumors with <200 cases reported in the literature [2, 3]. There is no specific clinical symptom, and most cases are discovered incidentally [4]. Abdominal discomfort can occur; some patients reported fever or asthenia [1, 4]. To our knowledge, this is the first reported case in Ecuador. In our case, she suffered abdominal pain and presented to the emergency room with acute abdomen. CT can help diagnose; SANT appears as low-density signals in the spleen with a clear boundary between the mass and the splenic parenchyma, as it was found in our patient [5, 6]. Magnetic resonance imaging or positron emission tomography scan can also be used to differentiate between malignant tumors; yet, because of their ability to grow, SANTs are often mistaken and are surgically resected [6]. Uterine clear cell carcinoma, colon cancer and rectal cancer should be in the differential [1, 7]. Due to their presentation, they should be treated as malignant lesions until the final diagnosis via pathology is achieved [8]. Pathological examination reveals a single or multiple white masses with a clear boundary from the surrounding splenic tissue [1, 3]. They are formed from various angiomatoid nodules fused together within a fibrous tissue of capillaries [2, 5]. Immunohistochemical stains reveal strong positivity for CD34. Nonetheless, they can also show positivity for CD31 and CD8, as it was discovered in our patient [1, 4].
In recent years the relationship between SANT and IgG4-related disease is under investigation. Many SANT patients show high blood levels of IgG4, and microscopically, some SANT lesions contain dense IgG4+ cells [6, 7]. Nonetheless, its relationships are yet to be determined [7]. Surgery is the treatment of choice, and splenectomy is needed [1, 4]. Laparoscopic or conventional approaches are available, and surgical oncologic principles should be followed [8]. A biopsy can be performed in the preoperative period. Nonetheless, the high risk of hemorrhagic complications during these procedures should be considered [2, 4]. As our patient presented with an acute abdomen and a splenic mass, surgery was completed without complications.
The incidence of overwhelming postsplenectomy infection should be analyzed by the surgical team, as it can be as high as 4.3% [1]. Therefore, immunizations for splenectomized patients should be given in all patients scheduled for elective splenectomy and during the postoperative period for urgent or emergent splenectomy patients, as it happened to our patient [1, 4].
When faced with a splenic lesion, it is critical to recognize the mass correctly; the relative rarity of splenic metastases and the uncommonness of SANT combined with the spleen’s fragility and the malignant potency of the splenic neoplasms make fast and accurate diagnosis a priority. This case highlights the importance of timely diagnosis and therapy in any tumor. When faced with a splenic mass, prompt treatment can change the patient’s prognosis. Nonetheless, as SANT is a sporadic tumor, more research is needed to clarify its pathogenesis and its prognosis.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



