-
PDF
- Split View
-
Views
-
Cite
Cite
Alhanouf Alhazzab, Ali Alkhaibary, Sami Khairy, Wael Alshaya, CLOVES syndrome and cervical arteriovenous fistula: a unique association managed by combined microsurgical and endovascular therapy, Journal of Surgical Case Reports, Volume 2021, Issue 4, April 2021, rjab122, https://doi.org/10.1093/jscr/rjab122
Close - Share Icon Share
Abstract
CLOVES syndrome is a condition characterized by congenital lipomatous overgrowth, vascular malformations, epidermal nevi and skeletal anomalies. The association of cervical arteriovenous fistula with CLOVES syndrome is extremely rare. To the best of our knowledge, only two cases were reported in the literature. We hereby report an additional case and review the literature on this condition. A 12-year-old girl, known to have CLOVES syndrome, presented to the emergency department with a 2-week history of bilateral, progressive lower extremity and left arm weakness. Radiological imaging demonstrated a C3–C6 left extradural lesion, containing multiple enhancing vessels, causing marked compression on the spinal cord. Urgent spinal decompression was performed, with C3–C6 instrumentation, followed by a two-stage embolization of the fistula. Cervical arteriovenous fistula can be rarely identified in patients with CLOVES syndrome. High index of suspicion is required to promptly evaluate patients with CLOVES syndrome presenting with new-onset neurological deficits.
INTRODUCTION
Congenital lipomatous overgrowth, vascular malformations, epidermal nevi, skeletal anomalies (CLOVES) syndrome is a rare a non-Mendelian genetic overgrowth disorder occurring sporadically [1, 2]. CLOVES syndrome is extremely rare, ~130–150 cases are currently living with the condition worldwide [1]. The syndrome is commonly characterized by complex truncal vascular malformation, bilateral overgrowth of the feet, and macrodactyly [1].
The identification of cervical arteriovenous fistula in patients with CLOVES syndrome is extremely rare. A review of the literature reveals two prior reported cases. Considering the rarity of cervical arteriovenous fistula in patients with CLOVES syndrome, we hereby outline the clinical presentation, radiological findings, surgical intervention and outcome of cervical arteriovenous fistula in a 12-year-old girl with CLOVES syndrome, as well as review the pertinent literature on this condition.
CASE REPORT
Clinical Data
A 12-year-old girl, known to have CLOVES syndrome diagnosed at birth, presented to the emergency department with a 2-week history of bilateral, progressive lower extremity and left arm weakness. The lower extremity weakness gradually worsened, resulting in imbalanced gait, with two episodes of accidental falls. The weakness was ascending in nature, affecting her left upper extremity. The patient reported moderate neck pain for the same duration. A systematic review of her history did not reveal any other associated neurological deficits.
Upon arrival to the emergency department, she was vitally stable, alert with a Glasgow coma scale (GCS) of 15/15. Her cranial nerves examination was normal. Visual fields were intact to confrontation with full extra-ocular movements. Power examination revealed bilateral lower extremity motor power of 4/5 over the hip, knee and ankle. Left upper limb motor power was 3/5 over the shoulder, elbow, wrist and hand muscles. Whereas on the right side, the motor power was 4/5 over the shoulder, elbow, wrist and hand muscles. Sensation was intact across all dermatomes. Babinski reflex was positive. Her gait was spastic in nature, slightly dragging both feet. With this initial presentation, the patient was admitted to the hospital for neuroradiological investigations and possible urgent surgical intervention to decompress the spinal cord.
Radiological images
Whole spine MRI showed a C3–C6 left extradural lesion causing marked compression on the spinal cord (Fig. 1). Cerebral angiography confirmed an arteriovenous fistula (Fig. 2).
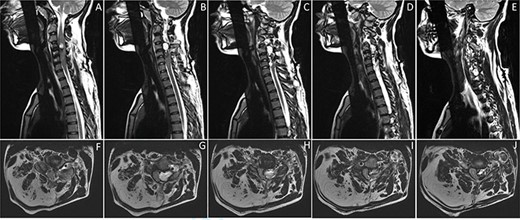
Sagittal (A-E) and axial (F-J) images of T2-weighted MRI of the cervical spine showing a left-sided extradural heterogeneously high T2-signal intensity lesion at C3–C6, causing compressing on the adjacent spinal cord. The lesion is containing multiple small vessels, extending through the left C4–C5 foramina. It measures 4.9 x 4.7 x 1.6 cm in maximum craniocaudal, transverse and anterior–posterior dimensions. The lesion is corresponding with arteriovenous fistula. There is evidence of bony outgrowth of C4 right facet join, contributing to the mass effect on the spinal cord. There is fat hypertrophy involving the posterior right neck, corresponding to the upper limb infiltrative lesion (F-J).

Cerebral angiography, with left vertebral artery injection, demonstrates evidence of arteriovenous shunting. The lesion is suggestive of arteriovenous fistula in the left upper cervical region. The arterial supply, from a hypertrophied branch of the left vertebral artery, was arising at the level of C2. However, the fistulous connection was at the level of C3 and C4.
Surgical intervention
Given the nature of progression of her status, the patient required urgent surgical intervention to decompress the spinal cord, with C3–C4, C4–C5, C5–C6 instrumentation. A posterior midline approach from the level of C2 to the level of C6 was performed. Screws were placed on C3, C4 and C5 vertebrae bilaterally and on the right side of C6 due to the loss of distracted process affecting the facet joint. Two rods were placed afterwards to complete the instrumentation. Following laminectomy, the lesion was visualized on the left side of the epidural space compressing the spinal cord. It had vascular appearance, resembling a venous pouch. The preliminary impression of an arteriovenous fistula was confirmed by intraoperative Doppler ultrasound, eliciting bruits inside the lesion.
Postoperative course
The patient was kept on a cervical collar and was started on physiotherapy program. Her neurological symptoms were maintained at baseline. There was a large venous pouch, as suspected intraoperatively, along the left side of the spinal canal draining into the upper cervical venous plexus (Fig. 2). Embolization of the fistulous connection was performed after selective catheterization of the branch of the left vertebral artery. After embolization, there was no evidence of residual arteriovenous shunting.
Outcome and follow-up
One month after admission, the patient was discharged with improvement in her clinical status. The patient is currently followed up in pediatric neurosurgery clinic with regular neuroradiological imaging.
DISCUSSION
Cervical arteriovenous fistula, in the setting of CLOVES syndrome, among the pediatric population is extremely rare. A review of the reported cases in the literature revealed only two cases of this unique association (Table 1). We herein report an additional case who underwent combined surgical and endovascular management at our institution.
Summary of the reported cases in the literature of cervical arteriovenous fistula in patient with CLOVES syndrome
| No. . | Author, Year . | Age/Sex . | Clinical presentation . | Fistula level . | Management . | |
|---|---|---|---|---|---|---|
| Endovascular . | Surgical . | |||||
| 1 | Boroumand et al. 2016 [5] | 54/F | Neck pain & myelopathy | C7–T2 | + | + |
| 2 | Hedequist et al. 2015 [7] | 4/F | Hemiplegia & gait disturbance | C2–C6 | + | + |
| 3 | Present case, 2021 | 12/F | Paresis & gait disturbance | C3–C6 | + | + |
| No. . | Author, Year . | Age/Sex . | Clinical presentation . | Fistula level . | Management . | |
|---|---|---|---|---|---|---|
| Endovascular . | Surgical . | |||||
| 1 | Boroumand et al. 2016 [5] | 54/F | Neck pain & myelopathy | C7–T2 | + | + |
| 2 | Hedequist et al. 2015 [7] | 4/F | Hemiplegia & gait disturbance | C2–C6 | + | + |
| 3 | Present case, 2021 | 12/F | Paresis & gait disturbance | C3–C6 | + | + |
M: male; F: female; C: cervical; NA: not available; (+): performed; (−): not performed.
Summary of the reported cases in the literature of cervical arteriovenous fistula in patient with CLOVES syndrome
| No. . | Author, Year . | Age/Sex . | Clinical presentation . | Fistula level . | Management . | |
|---|---|---|---|---|---|---|
| Endovascular . | Surgical . | |||||
| 1 | Boroumand et al. 2016 [5] | 54/F | Neck pain & myelopathy | C7–T2 | + | + |
| 2 | Hedequist et al. 2015 [7] | 4/F | Hemiplegia & gait disturbance | C2–C6 | + | + |
| 3 | Present case, 2021 | 12/F | Paresis & gait disturbance | C3–C6 | + | + |
| No. . | Author, Year . | Age/Sex . | Clinical presentation . | Fistula level . | Management . | |
|---|---|---|---|---|---|---|
| Endovascular . | Surgical . | |||||
| 1 | Boroumand et al. 2016 [5] | 54/F | Neck pain & myelopathy | C7–T2 | + | + |
| 2 | Hedequist et al. 2015 [7] | 4/F | Hemiplegia & gait disturbance | C2–C6 | + | + |
| 3 | Present case, 2021 | 12/F | Paresis & gait disturbance | C3–C6 | + | + |
M: male; F: female; C: cervical; NA: not available; (+): performed; (−): not performed.
It is noteworthy to mention that CLOVES syndrome was first described in 2007 by Sapp et al. [3] in a cohort of seven patients. Those patients were initially thought to have Proteus syndrome, a condition characterized by postnatal, progressive, asymmetric overgrowth [1, 3, 4]. However, those patients were not meeting the diagnostic criteria of Proteus syndrome [3]. Due to the distinctive natural history of CLOVES syndrome from that of Proteus syndrome, the condition was established and subsequently gained its nomenclature [3]. Unlike Proteus syndrome, CLOVES syndrome tends to be congenital, presenting prenatally or at birth [1]. Cardinal features of CLOVES syndrome include the proportional growth with the patient and the bilateral involvement of the feet [4].
To date, the exact etiology of CLOVES syndrome remains uncertain [5]. However, somatic mosaic mutation, in PIK3CA gene, occurring early in the embryogenesis phase was postulated to explain CLOVES syndrome [2]. This was evident by performing DNA and RNA sequencing of the affected tissues in patients with CLOVES syndrome [2].
The association of shunts with fatty tissue overgrowth may propose a link between endothelial cells and adipocytes during embryogenesis [5]. Rupnick et al. [6] concluded that the growth of adipose tissue is angiogenesis-sensitive and can be regulated via different angiogenesis inhibitors. The patient in the present case had fat hypertrophy in her posterior neck, which may possibly suggest the association of the fistula with fat hypertrophy.
Boroumand et al. [5] reported the first case of combined surgical and endovascular management of arteriovenous fistula in an adult patient with CLOVES syndrome. The patient underwent endovascular and microsurgical management, in an attempt to disconnect the complex arteriovenous fistula [5]. The patient in the present case underwent similar management, comprising surgical decompression and staged embolization of the fistula.
CONCLUSION
Cervical arteriovenous fistula can be rarely encountered in patients diagnosed with CLOVES syndrome. A high index of suspicion is required to identify patients with CLOVES syndrome presenting with new-onset neurological deficits. In experienced neurosurgical centers, combined surgical and endovascular management of the fistula can be considered to prevent permanent neurological sequalae. A multidisciplinary approach, utilizing neuro-interventional and microsurgical techniques, provides high-quality care to patients with CLOVES syndrome harboring cervical arteriovenous fistula.
CONFLICT OF INTEREST STATEMENT
The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
FUNDING
None.



