-
PDF
- Split View
-
Views
-
Cite
Cite
Yuki Horio, Motoi Uchino, Takako Kihara, Toshihiro Bando, Ryuichi Kuwahara, Tomohiro Minagawa, Kurando Kusunoki, Kenji Watanabe, Seiichi Hirota, Hiroki Ikeuchi, Potential problems of partial resection for colitis-associated cancer in a patient with ulcerative colitis: case report, Journal of Surgical Case Reports, Volume 2021, Issue 3, March 2021, rjab086, https://doi.org/10.1093/jscr/rjab086
Close - Share Icon Share
Abstract
Total proctocolectomy and an ileal pouch-anal anastomosis are recommended as the standard procedure for ulcerative colitis (UC)-colitis-associated cancer (CAC). However, several studies have reported the partial colectomy and endoscopic resection of UC-CAC in recent years. We present a surgical case of UC-CAC that was detected at a site that had not been diagnosed preoperatively, and we report potential problems of partial colectomy and endoscopic resection through this case. Considerations of synchronous and metachronous cancer/dysplasia are important before partial resection is planned for CAC in UC. Moreover, it should be noted that endoscopic resection at the anal site can be a risk factor for pouch surgery failure due to fibrosis after resection.
INTRODUCTION
Ulcerative colitis (UC) is steadily increasing in Japan due to the aging of the population and the increase in the number of long-term patients caused by the progress of medical treatment. The number of patients who require surgery for colitis-associated cancer (CAC) is also increasing [1]. Total proctocolectomy and an ileal pouch-anal anastomosis (IPAA) are recommended as the standard procedure for UC-CAC/high-grade dysplasia [2]. Conversely, several studies have reported the partial resection and curative endoscopic submucosal dissection (ESD) of neoplasms in UC, and surveillance colonoscopy is recommended after complete removal via endoscopic resection [3, 4]. However, there are still many problems, such as the lack of long-term outcomes and the difficulty of the procedure.
We report a case of UC-CAC that was detected at a site that had not been diagnosed preoperatively.
CASE
A 56-year-old man was diagnosed with UC at the age of 30. He was controlled with 5-aminosalicylic acid and enemas and was treated with prednisolone at the time of exacerbation. He underwent regular surveillance endoscopy. At the age of 56, the patient was in remission. An Isp-type lesion was detected on the lower rectum, and it was diagnosed as group 5. Endoscopic findings are shown in Fig. 1. Isp-type lesions were found in the lower rectum near the dentate line. There were no findings of cancer in other sites of the pan-colon by surveillance endoscopy. Endoscopic mucosal resection (EMR) was tried to distinguish between sporadic cancer and CAC. Although the negative nonlifting sign was confirmed, EMR could not be performed due to the difficulty of snaring. Finally, the patient was recommended to choose ESD or surgery. Therefore, he was referred to our department for surgery at his own will.
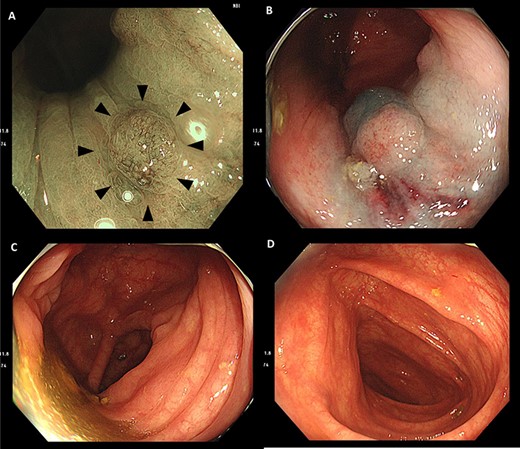
(A) Endoscopic findings indicated Isp-type lesions in the lower rectum (arrowhead). (B) It was difficult to secure adequate margins by snaring during endoscopic mucosal resection due to contact with the dentate line. (C and D) There were no findings of cancer in ascending colon.
The physical findings on admission were as follows: blood pressure 129/70 mmHg, pulse 72 times/min, body temperature 37.3°, stool frequency 1–2 times/day and no bloody stools. The blood biochemical test findings indicated a hemoglobin level of 13.1 g/dl and an erythrocyte sedimentation rate of 5 mm (1 H), which was normal. The UC severity was mild by using the criteria of Truelove and Witts [5]. The disease extent of UC was pancolitis. Tumor markers were normal: carcinoembryonic antigen: 1.1 ng/ml and carbohydrate antigen 19-9: 10.4 U/ml. By computed tomography, tumors could not be identified, and multiple diverticula were found in the ascending colon, descending colon and sigmoid colon. No other obvious abnormalities were observed, and no metastatic lesions were found.
The patient underwent laparoscopic-assisted total proctocolectomy, mucosectomy, handsewn IPAA and ileostomy construction. The surgical findings were no ascites and no obvious metastatic lesions. The resected specimen is shown in Fig. 2.

The resected specimen shows a 15 × 14 mm Ip lesion that was found in the ascending colon (arrow head), and a 5 mm-sized elevated lesion was observed in the lower rectum (dotted line circle): it is difficult to recognize with the naked eye.
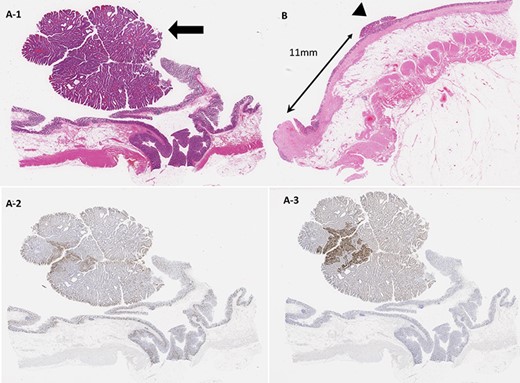
(A-1) Histopathological findings. A 15 × 14 mm Ip lesion was found in the ascending colon, and a well-differentiated tubular adenocarcinoma showing moderate atypia was found in the tubular lineage (arrow). (A-2) Ki-67 was highly positive, whereas p53 was strongly positive in a diffuse manner. (A-3) p53 was weakly positive in a mosaic pattern and in the cancerous component. (B) In the lower rectum, a 5 mm-sized elevated lesion was observed, and a low-grade dysplasia-equivalent image showing moderate atypia was also obtained (arrowhead). The resected margin, which was 11 mm in size, was negative.
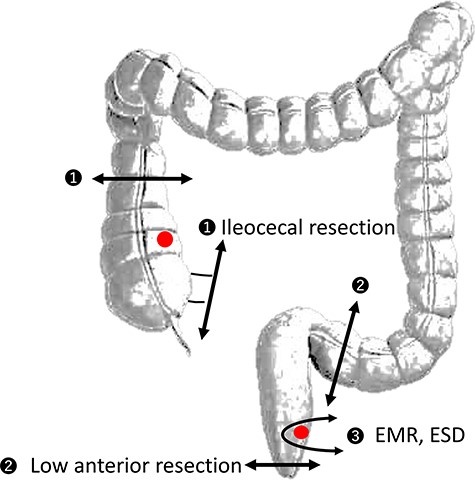
Potential problems of segmental colectomy and endoscopic treatment ❶ Metachronous cancer after ileocecal resection: small intestine and mesentery adhesions to the right retroperitoneum that make creating the pouch and reaching the anus difficult❷ Metachronous cancer after low anterior resection makes future pouch surgery difficult owing to adhesion or pelvic infection❸ Postendoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) in the surgical anal canal These procedures lead to surgical anal canal fibrosis and stenosis, and surgeons may encounter difficulties with mucosectomy and insertion of the circular stapler.
The histopathological findings were as follows: a 15 × 14 mm Ip lesion was found in the ascending colon, and a well-differentiated tubular adenocarcinoma showing moderate atypia was found in the tubular lineage. In the lower rectum, a 5 mm-sized elevated lesion was observed, and a low-grade dysplasia-equivalent image showing moderate atypia was also obtained. The resected margin, which was 11 mm in size, was negative. No lymph node metastasis was observed (Fig. 3). The 8th Union for International Cancer Control Pathological TNM staging system classification was A, 0-Ip, tub1, pTis (M), ly0, v0, pN0 (0/11), pPM0, pDM0 and stage 0.
DISCUSSION
Total proctocolectomy is recommended as the standard procedure for UC-CAC/high-grade dysplasia in the Japan guidelines, ECCO guidelines and practice parameters of the American Society of Colon and Rectal Surgeons [2, 6, 7]. Partial resection and ileorectal anastomosis have limited indications [8, 9]. The reasons include the risks of a high frequency of multiple cancer lesions and the development of CAC in the remnant colon [10]. Regarding synchronous cancer, Hata et al. [11] reported that 17 out of 238 (7.14%) cases with invasive CAC were unrecognized preoperatively. For these cases, it was not enough just to perform a partial resection, and they required reoperation immediately. Regarding metachronous cancer, there is no evidence of long-term outcomes for metachronous UC-CAC after segmental resection. Even if we detect synchronous cancer reliably and we perform a partial resection, there is no guarantee that metachronous cancer can be detected after surgery. In addition, the kind of surgery that can be performed in the reoperation becomes a further problem. The most common sites of UC-CAC are the rectum and sigmoid colon, and therefore, the performance of several repeated pelvic surgeries would probably make future pouch surgery difficult owing to adhesion or pelvic infection.
Regarding endoscopic treatment for dysplasia, the SCENIC statement of the international consensus meeting held in 2014 stated, ‘After complete removal of endoscopically resectable dysplastic lesions, surveillance colonoscopy is recommended rather than colectomy’ [12]. However, there are many problems, such as that the definition of endoscopically resectable lesions has not been determined, the procedure is difficult due to submucosal fibrosis and the long-term outcome is still unclear. With this assumption, accurate diagnosis is a prerequisite for performing endoscopic treatment. In the present case, ascending colon cancer that was not diagnosed before surgery was detected during the pathology analysis of an excised colorectal specimen. In addition, if there is anal transition zone cancer, endoscopic diagnosis and treatment will be difficult. Even if either EMR or ESD was performed, these procedures lead to surgical anal canal fibrosis and stenosis, and surgeons may encounter difficulties with mucosectomy and insertion of the circular stapler.
Although there are several reports recommending partial recession, EMR and ESD, these procedures should not be taken for granted, as there is still low-grade evidence. In this case report, the physicians had to determine the treatment strategies considering various issues such as unrecognized synchronous cancer, metachronous cancer and future surgical plans. We summarized these potential problems in a schema (Fig. 4).
Considerations about synchronous and metachronous cancer/dysplasia are important before the planning of partial resection for CAC in UC. Moreover, it should be mentioned that endoscopic resection at the anal site can be a risk factor for failure of IPAA due to fibrosis after resection.
AUTHORS’ CONTRIBUTIONS
Y.H. drafted the article. Y.H., T.B., R.K., T.M. and K.K. treated and observed the patient. K.H. and S.H. carried out the histopathological diagnosis. M.U., K.W. and H.I. contributed towards drafting the article or revising it critically for important intellectual content and providing final approval. All authors have read and approved the manuscript.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
CONFLICT OF INTEREST
None declared.
FUNDING
None declared.
ABBREVIATIONS
IPAA, ileal pouch-anal anastomosis; UC, ulcerative colitis; CAC, colitis-associated cancer; EMR, endoscopic mucosal resection; ESD, endoscopic submucosal dissection.



