-
PDF
- Split View
-
Views
-
Cite
Cite
Annalise Bellizzi, Reuben Vella Baldacchino, Fawz Kazzazi, Parto Forouhi, Charles M Malata, The successful use of disparate pedicle types for bilateral therapeutic mammaplasties during breast conservation surgery, Journal of Surgical Case Reports, Volume 2021, Issue 3, March 2021, rjab064, https://doi.org/10.1093/jscr/rjab064
Close - Share Icon Share
Abstract
This case illustrates the successful use of non-identical pedicles in bilateral therapeutic mammaplasty (TM). A 58-year-old patient presented with a left-sided upper inner quadrant multifocal invasive [no special type (NST)] tumour and a right-sided upper outer quadrant unifocal invasive tubular carcinoma with surrounding ductal carcinoma in situ (DCIS). Her tumour locations necessitated simultaneous bilateral TM using different pedicle types. A superomedial pedicle T-scar breast reduction was undertaken on the right to resect the upper outer quadrant tumour whilst a superolateral nipple transposition pedicle was used on the left breast to enable the wide resection of the two tumours located superomedial to the nipple. The location and size of the tumour also required the use of a secondary infero-medially based pedicle for volume displacement on the left breast. Patient received adjuvant chemotherapy and radiotherapy. A year after surgery the patient has acceptable cosmetic results in terms of symmetry, breast contour and increasingly inconspicuous scars.
INTRODUCTION
Therapeutic mammaplasty (TM) is a well-described technique for the treatment of some breast cancers. Its principal objectives are to avoid mastectomies whilst maintaining cosmetic results and improving the breast shape and contour. It is associated with improvement of symptoms of macromastia and often patients look better post-operatively than pre-operatively [1].
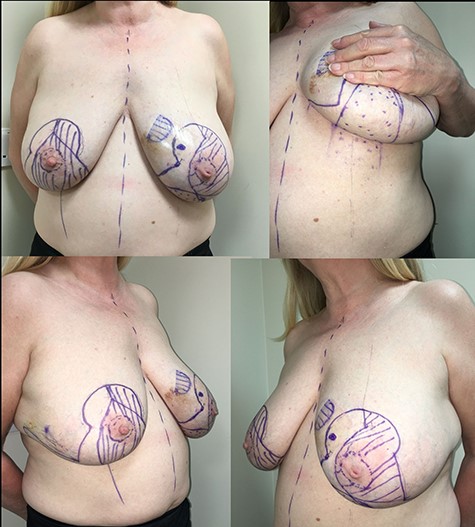
Pre-operative markings. Bilateral-Wise pattern skin reduction markings, showing anterior, oblique and inferior views. Note is made of significant size asymmetry between right and left breast.
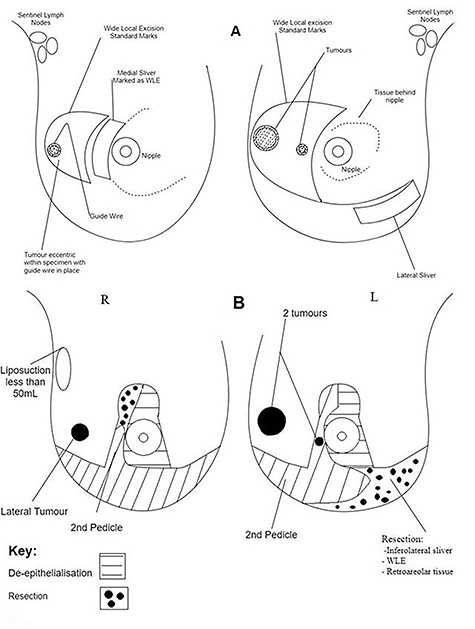
Operative diagrams. (A) Breast surgeon’s operative diagram; (B) plastic surgeon’s operative diagram.
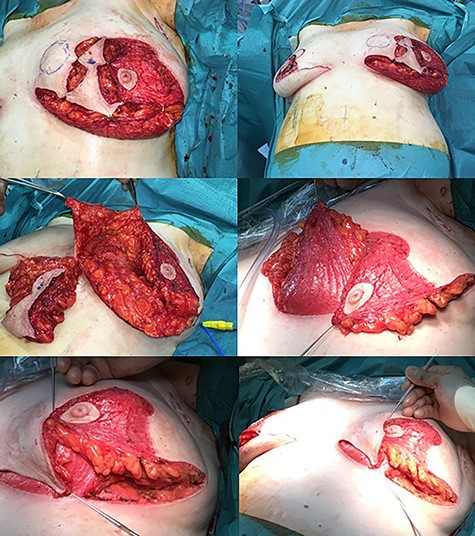
Intraoperative photographs of the left breast. Resection and tissue rearrangement was more complex needing a secondary (totally de-epithelialised) infero-medial dermoglandular pedicle in addition to a supero-lateral nipple-carrying dermoglandular pedicle. A standard superomedial pedicle was used for the right breast (not shown here).

Post-operative cosmetic results. Almost a year postoperatively, the radiotherapy side effects settled and she has great cosmetic results because reasonable symmetry was obtained and the breasts look natural. The scars are inconspicuous, and there has been no evidence of fat necrosis so far.
Traditionally, to achieve these objectives a balancing breast reduction is performed on the opposite breast. This invariably utilizes an identical pedicle as used for the contralateral TM. The main reason for this is that the use of different pedicles can result in poor cosmetic results especially with regard to symmetry.
We present a patient with bilateral breast cancer undergoing bilateral breast conserving surgery (BCS) who by virtue of her tumour locations required simultaneous bilateral therapeutic mammaplasties (TMs) using completely different pedicle types.
CASE REPORT
A 58-year-old patient presented with left-sided upper inner quadrant multifocal invasive no special type (NST) tumours and right-sided upper outer quadrant unifocal invasive tubular carcinoma with surrounding ductal carcinoma in situ (DCIS).
Examination revealed large, heavy, pendulous breasts with significant size asymmetry (38EE cup-size; with the left breast being much larger than the right). The diagnosis was established using standard triple assessment and in addition, an MRI was performed. The MRI showed two lesions 14 mm apart measuring 36 × 21 and 16 × 12 mm in the left breast, both of which were malignant and appeared to be bridged. It also revealed a small irregular lesion measuring 16 × 8 mm in the upper outer quadrant of the right breast. The final pre-treatment TNM staging was T2N0M0 on the left and T1bN0M0 on the right. Breast core biopsy revealed the left tumours to be grade 3 invasive NST and the right being a grade 1 invasive tubular carcinoma, both were ER positive and PR/HER 2 negative.
Because of the reasonably large sizes of the tumour complex relative to breast, a left mastectomy was discussed but the patient expressed a strong preference for BCS. Given the relatively large size of the breasts (38EE), the multi-disciplinary team decided that this was an acceptable course of action. Bilateral-Wise pattern skin reduction markings were made prior to surgery (Fig. 1). She underwent bilateral wide local excisions and bilateral sentinel lymph node biopsies (SLNB). The SLNB on the left was performed through a separate incision to minimize the risk to the blood supply of the superolateral pedicle. A superomedial T-scar breast reduction was performed on the right breast to enable resection of the lateral tumour and a left superolateral breast reduction to enable the wide resection of the two tumours, which were located superomedial to the nipple.
Due to the large resultant superomedial defect created she also required the use of a secondary totally buried infero-medially based pedicle for volume displacement on the left breast (Figs 2 and 3). Post-operatively, there were no early problems. Histology showed tumour clearance by 15-mm margins on the right breast and 10 mm on the left.
She received 18 weeks of adjuvant chemotherapy using a third-generation regime, followed by adjuvant radiotherapy given as 40 Gy in 15 fractions over 3 weeks to both breasts and a left tumour bed boost of 12Gy in four fractions over 4 days. This caused transient skin effects.
She is currently on the local post-treatment surveillance programme. A year after surgery, she remains disease-free with a normal mammogram. The patient has excellent size and contour symmetry and is very satisfied with her cosmetic outcome (Fig. 4).
DISCUSSION
This case herein described illustrates the versatility of the Wise pattern technique in its use with different nipple pedicles, especially in the management of patients with large ptotic breasts. The Wise pattern enabled the use of different pedicles.
The superomedial technique is well described and is highly versatile [2]. The use of the Wise pattern reduction technique together with the superomedial pedicle is valuable for its applicability in yielding consistent and lasting cosmetic outcomes in various circumstances (i.e. tumour sizes and locations). This combination allows for larger breast reductions with improved breast contour whilst preserving excellent blood supply to the nipple and skin flaps. The superolateral pedicle, although used less often, is ideal for tumours located on the medial side [3]. Both pedicles are suitable for tumours in the lower quadrants.
This case highlights the importance of versatility in plastic and oncoplastic breast surgeons’ approach to performing TMs and novelly utilizing pedicles for atypically located lesions. The main use of the superolateral pedicle TM is in the treatment of medial and upper inner tumours. The defect left after resection of an upper inner tumour is challenging to fill in order to avoid a poor aesthetic result at this cosmetically sensitive site. However, the use of a superolateral pedicle in addition to an inferomedially based totally buried secondary dermoglandular pedicle to repair this defect achieved excellent aesthetic outcomes as reported in our case. It is an effective technique with good, reproducible cosmetic outcomes [4], and its use can be applied to a diversity of breast shapes and skin excision patterns whilst conferring improved superior pole fullness and breast projection. In addition, superolateral pedicles safeguard both nipple sensation and vascularity of the breast.
Inferior, lateral and upper outer tumours can be treated with a superomedial based pedicle reduction. For upper outer tumours, as in our case, the combination of the superomedial based pedicle with Wise pattern incision provides better access than a vertical incision due to the lateral position of the tumour. The superomedial pedicle is widely used given its advantages including shorter operation times, improved superior pole fullness and its low likelihood of causing pseudoptosis—a feature shared with superolateral pedicles [5]. It can be used for a wide array of skin incisions, breast shapes and sizes to achieve excellent long-term results.
This case illustrates that it is possible to use non-identical pedicles in bilateral TMs and highlights the importance of the surgeons being versatile. Unlike in cosmetic breast reduction, TM makes it possible to achieve cancer clearance and adequate cosmetic results even with the use of different pedicles.
CONFLICT OF INTEREST
This manuscript has neither been published, nor is being considered for publication elsewhere. This case report was presented as a poster at the BAPRAS Celtic Plastic Surgeons Meeting Dunkeld, Scotland, 8–9 November 2018.
FUNDING
None of the authors have a financial interest in any of the products, devices or drugs mentioned in this manuscript. No funding was obtained for this submission.
References
Blondeel PN, Hamdi M, Van de Sijpe KA, Van Landuyt KH, Thiessen FE, Monstrey SJ.



