-
PDF
- Split View
-
Views
-
Cite
Cite
Paolo Gasparella, Georg Singer, Christoph Arneitz, Martin Benesch, Erich Sorantin, Eva Kampelmühler, Peter Schemmer, Holger Till, Rapidly involuting congenital hemangioma of the liver in a newborn with incomplete Pentalogy of Cantrell: description of a new association, Journal of Surgical Case Reports, Volume 2021, Issue 3, March 2021, rjab047, https://doi.org/10.1093/jscr/rjab047
Close - Share Icon Share
Abstract
The perinatal management of newborns with giant omphaloceles requires careful suspicion concerning ‘unexpected’ associated malformations. We describe a newborn with a combination of incomplete Pentalogy of Cantrell consisting of giant omphalocele, anterior congenital diaphragmatic hernia (CDH) and pericardial absence complicated by a hepatic rapidly involuting congenital hemangioma (RICH). A giant omphalocele was detected prenatally. Postnatally, staged closure of the omphalocele was planned. A mass of the liver was noted and (mis-)taken for a hematoma. In the further course, the baby developed cardiorespiratory insufficiency due to a central CDH which was excised. Subsequently, staged closure of the omphalocele became impossible. Specific workup revealed a mass in the left liver lobe. The mass was resected and the abdominal wall defect repaired. Histology confirmed the diagnosis of an RICH. The surgical treatment of newborns with giant omphaloceles requires a multidisciplinary neonatal support and an elaborate pediatric surgical armamentarium to cope with additional malformations.
INTRODUCTION
The postnatal treatment of patients suffering from giant omphalocele is challenging due to the necessity to preserve the fragile balance between abdominal pressure and breathing dynamics during abdominal wall closure [1]. The degree of difficulty increases if the omphalocele is part of a more complex malformation like Pentalogy of Cantrell, a rare failure of embryonal closure of the anterior midline characterized by a combination of defects of the heart, pericardium, diaphragm, sternum and anterior abdominal wall [2]. Accurate diagnosis and closure of the defects represent the therapeutic milestones.
Most of the hepatic tumors diagnosed in the perinatal period are infantile hemangiomas (IHs) [3], but in rare cases, congenital hemangiomas (CHs) occur [4].
Herein, we describe a yet unreported combination of an incomplete Pentalogy of Cantrell consisting of giant omphalocele, anterior congenital diaphragmatic hernia (CDH) and pericardial defect complicated by the presence of a rapidly involuting congenital hemangioma (RICH) of the liver.
CASE REPORT
During a routine prenatal ultrasound screening in the 11th gestational week (GW), a 39-year-old woman was diagnosed with a fetus having a giant omphalocele containing almost the entire liver. MRI in the 30th GW confirmed the diagnosis of a covered abdominal wall defect and was negative for associated malformations.
In the 37th GW, caesarean section was performed. At birth, the male neonate presented a covered abdominal wall defect of 7 cm mostly occupied by the liver. An abdominal and cardiac ultrasound ruled out major associated malformations. The boy was scheduled for a staged closure. During surgery, a mass in the left liver was noted and (mis-)taken for a hematoma. A fascial Gore-Tex patch measuring 5 × 5 cm was applied.
On the 31st postnatal day, the patient’s general condition progressively worsened. Echocardiographic examinations showed worsening of the cardiac biventricular function due to herniation of the right liver into the chest. On Day 38 of life, closure of the anterior diaphragmatic hernia through the abdominal wound was performed. After reduction of the liver and resection of the CDH sac, absence of the pericardium was noted. The diaphragmatic defect of 5 × 4 cm was closed with a Gore-Tex patch and the abdominal wall defect was covered with a Gore-Tex (Fig. 1).
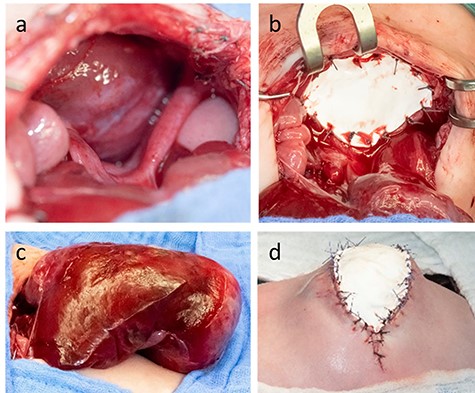
The anterior thoracic defect (a) was covered with a Gore-Tex-Patch (b). After mobilization from the anterior mediastinal space, the liver assumed an irregular shape not allowing abdominal wall closure (c). The defect was temporarily covered by a skin Gore-Tex -Patch (d).
In the following 3 weeks, staged closure was continued without much progress, mostly because of the lesion in the left liver. Work-up of this lesion by ultrasound and MRI demonstrated a 5.5 × 5.1 × 5.5 cm tumor in segment III of the liver consistent with the diagnosis of a vascular tumor. The attempted therapy with propranolol (1 mg/kg/day) was ineffective and was discontinued due to the onset of bradycardia. Finally, surgical resection of the liver tumor was decided. At surgery, the well-defined mass was completely resected (Fig. 2). While the abdominal fascia was closed using a Gore-Tex patch of 3 × 4 cm, the skin was closed directly.
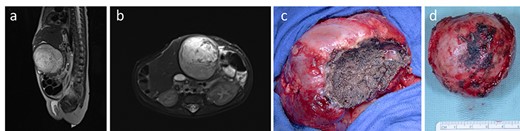
MRI showing the vascularized tumor originating from the liver, occupying the precaval space and protruding outside the abdominal wall level (a, b). At surgery, a cleavage sheet between liver and the mass (c) allowed an easy and complete resection of the tumor (d)
Pathological examination showed a mass enclosed by a capsule of about 2 mm and containing a marginal area rich in a dense network of capillary vessels and a central necrotic region. Immunohistochemical examination was positive for endothelial markers CD31 and CD34, and negative for GLUT1. The proliferation rate under 5% and the sequencing of GNA-11 mutation made the diagnosis of RICH the most appropriate.
The postoperative course was uneventful and the patient was discharged home on the 29th postoperative day at the age of 3 months. No recurrences were noted at the last follow-up at 8 months.
DISCUSSION
Herein, we report a case of a postnatal diagnosis of incomplete Pentalogy of Cantrell complicated by a vascular liver tumor successfully treated by a multidisciplinary team.
Following description of the association of five midline defects termed Pentalogy of Cantrell [5], several authors have reported incomplete forms in which, similar to our patient, at least three of them are present [6].
The prenatal diagnosis of a giant omphalocele can represent a first warning sign of Pentalogy of Cantrell. In cases with associated cardiac anomalies, prenatal MRI is recommended [7]. In our patient, however, Pentalogy of Cantrell was not suspected prenatally due to the lack of a large cardiac malformation.
The presence of a diaphragmatic and an abdominal defect are a particular challenge for pediatric surgeons. Maintaining a low intraabdominal pressure is necessary to guarantee efficacious respiratory mechanics. The alteration of this delicate balance is responsible for the mortality of one-fifth of patients with giant omphaloceles [8]. Therefore, multi-staged closure approaches consisting of the application of patches have been proposed, with the goal to allow time for the abdominal wall to adapt [1]. In our case, we initially opted for a temporary closure of the abdominal wall using a synthetic patch.
The occurrence of a hepatic tumor in the first months of age, which complicated the abdominal wall closure in our patient, is rare and in most cases consists of vascular tumors, mesenchymal hamartomas or hepatoblastomas [3]. In particular, hepatic vascular tumors show distinctive features. Hepatic IHs usually appear after birth and may cause cardiac failure during its proliferative phase. Conversely, CHs develop during pregnancy and are fully developed at birth. According to their subtype involution can be rapid, partial or absent [9]. In our patient, the absence of the lesion in the prenatal MRI initially suggested the diagnosis of IH, for which the first-choice therapy is propranolol. In our case, this treatment did not induce any decrease of tumor volume, and therefore, resection of tumor was scheduled.
In most cases, the diagnosis of hepatic CH is incidental and simple observation seems to be the best option. The particular challenge of the present case consisted in the size and the localization of the CH which occupied the whole space between the opened abdominal wall superiorly and the major abdominal vessels inferiorly. We opted to remove the tumor in order to have a histopathological diagnosis and also to facilitate abdominal wall closure.
In conclusion, the occurrence of an incomplete Cantrell Pentalogy in association with an RICH has not been reported yet. Resection of the tumor facilitated the closure of the abdominal wall and the patient shows an event free follow-up at 8 months.
FUNDING
None.
PROPRIETARY INTEREST STATEMENT
The authors declare that they have no relevant or material financial interests that relate to the research described in this manuscript.
STATEMENT
The patient’s family agreed in writing to publish the reported photographic documentation.
References
- pericardial sac
- congenital abnormality
- hematoma
- infant
- newborn
- pediatrics
- surgical procedures, operative
- diagnosis
- histology
- liver
- omphalocele
- abdominal wall defect
- hernia, congenital diaphragmatic
- pentalogy of cantrell
- congenital hemangioma, rapidly involuting
- perinatal period
- liver lobe
- newborn care management



