-
PDF
- Split View
-
Views
-
Cite
Cite
Raed AlAsmi, Mohammed Alfozan, Page kidney post ureteroscopy: a case report, Journal of Surgical Case Reports, Volume 2021, Issue 2, February 2021, rjab021, https://doi.org/10.1093/jscr/rjab021
Close - Share Icon Share
Abstract
Renal injury after surgical intervention is not uncommon in current urological practice with most complication would be anticipated in high risk patient. Subcapsular renal hematoma is not known complication post some urological interventions such as extracorporeal shockwave lithotripsy (ESWL), percutaneous nephrolithotomy (PCNL) and trauma. Few cases of subcapsular hematomas are reported as a complication post ureteroscopy in the literature. Clinical spectrum varies from spontaneous resolution through acute renal failure secondary to Page kidney. Page kidney is the external compression of a kidney usually caused by a subcapsular hematoma associated with high blood pressure and occasional renal failure. It is named after Dr. Irvin Page who first demonstrated in 1939 that applying external compression on the renal parenchyma could cause hypertension. Various management options are mentioned in literature and depend upon the severity and presentation. Percutaneous drainage is an option for the management of subcapsular hematoma in hemodynamically stable patient.
INTRODUCTION
Subcapsular renal hematoma is known complication of extracorporeal shockwave lithotripsy (ESWL), trauma, interventional procedure or rarely spontaneously in some patients with malignancy. Clinical presentation varies from asymptomatic to acute renal failure and Page kidney. Few cases of symptomatic subcapsular hematoma post ureteroscopy are reported in the literature.
We report a case of acute renal failure secondary to subcapsular renal hematoma post ureteroscopy.
CASE PRESENTATION
A 35-year-old male, known case of solitary kidney post donor nephrectomy to a relative 3 years ago, presented to the emergency department with 3 days history of anuria with right flank pain, shortness of breath and generalized edema.
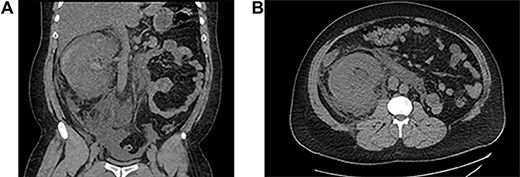
He underwent ureteroscopy and removal of ureteric stent which was inserted 3 weeks ago for an upper ureteric radiolucent stone in another hospital. The patient did not report passing the stone but ureteroscopy was negative. During his recovery after ureteroscopy and stent removal the patient developed right flank pain on Day 1 postoperative and presented to initial hospital, and was discharged from the emergency department on oral analgesics. On the third day he presented to our hospital with anuria and shortness of breath and generalized edema. His laboratory finding showed creatinine level at presentation was 735. Computed tomography (CT) abdomen without contrast showed a subcapsular hematoma with mild hydronephrosis (Fig 1). The patient was taken for percutaneous drainage using 8 Fr nephrostomy tube which drained hematouric urine with clots of 1.5 L (Fig. 2). Post drainage the patient had good urine output and the creatinine level dropped to 492. He was monitored for possible postobstructive diuresis which was anticipated and managed. He recovered his renal functions and creatinine level went back to normal levels with good urine output. On the third day the nephrostomy tube was clamped, and the patient was voiding freely with no flank pain or leak. The nephrostomy tube was removed, and he was discharged. A follow-up CT after 1 month showed complete resolution of the hematoma and the renal profile was normal.

Antegrade pyelogram post drainage and insertion of nephrostomy tube.
DISCUSSION
Subcapsular renal hematomas are usually related to kidney trauma and are well-known complications of ESWL [2]. The causes of spontaneous hematoma include tumors, vascular diseases, infections, cystic diseases, hydronephrosis, preeclampsia and blood dyscrasias [3]. Few cases of subcapsular hematoma post ureteroscopy reported in the literature.
The etiology of the subcapsular renal hematoma after URSL has remained unclear. The recent report speculated that the most probable explanation for the development of subcapsular hematoma could be trauma to the pelvicalyceal system during guide wire manipulation or raised intrarenal pressure leading to forniceal rupture and separation of the capsule from the parenchyma and hematoma [1]. Some diseases increase the risk of developing subcapsular hematoma such as diabetes, hypertension and infection due to pathological changes in the renal parenchyma. Bai et al. [4] showed that larger stone size, severe hydronephrosis, increased surgical time and higher perfusion pressure of hydraulic irrigation were risk factors which are significantly associated with the development of subcapsular renal hematoma.
The clinical presentation of these patients varies considerably based on the degree and duration of the bleeding. Acute onset of flank or abdominal pain is the most common symptom. Other patients may present with hematuria, a palpable mass, signs of blood loss [3] or anuria in case of bilateral hematoma or solitary kidney.
A percutaneous drainage, laparoscopic decortication may be done to decrease surgical aggressiveness in patients with stable vitals but with unbearable pain or renal compression [2, 5]. If hematoma is rapidly progressive or the vitals are deteriorating, conventional drainage by open surgery may be performed [2].
We preferred to relieve the pressure by percutaneous drainage and our patient responded well with rapid recovery of renal function.
CONCLUSION
Although subcapsular hematoma post ureteroscopy is a rare complication, the physician should have high index of suspicion when patient present with severe flank pain, fever and oliguria/anuria post ureteroscopy.
CONFLICT OF INTEREST STATEMENT
There is no conflict of interest.
SOURCE OF SUPPORT
None.



