-
PDF
- Split View
-
Views
-
Cite
Cite
Shivani Angelique Kumar, Connor O’Meara, Sue Fredericks, Thomas Havas, Beware the respiratory epithelial adenomatoid hamartoma—a malignant masquerador, Journal of Surgical Case Reports, Volume 2021, Issue 2, February 2021, rjab007, https://doi.org/10.1093/jscr/rjab007
Close - Share Icon Share
Abstract
Respiratory epithelial adenomatoid hamartoma (REAH) is a rare benign tumour, which can masquerade as a sinonasal malignancy. Commonly arising from the posterior nasal septum, we present the second described case of a lateral nasal cavity wall REAH in a 68-year-old male with a 2-year history of progressive left nasal obstruction. Clinical and radiological assessment predicted malignancy; however, histopathology identified a benign pathology. He was subsequently treated with narrow local excision under general anaesthetic with no evidence of recurrence at post-operative intervals.
INTRODUCTION
Hamartomas are predominately benign tumours [1, 2], a local malformation of multiple aberrant cell types, rather than a single mutated cell proliferation [1, 3]. Respiratory epithelial adenomatoid hamartoma (REAH) arises from Schneiderian respiratory epithelium (pseudostratified respiratory epithelium), the surface epithelium within nasal cavity and sinonasal space [2, 4, 5].
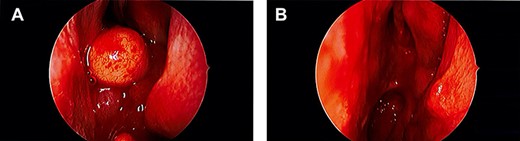
Intraoperative endoscopic images. (A) Large, spherical, well-circumscribed polypoidal tumour in the left nasal passage; (B) post-operative image showing complete excision of the lesion.
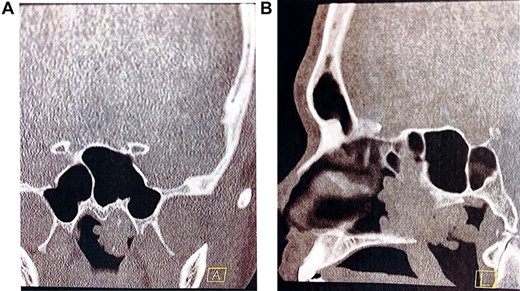
Pre-operative computed tomography of the nasal passage and sinuses. (A) Coronal CT sinuses (bone algorithm) demonstrating left nasopharyngeal space ‘polypoid’ type opacification, with evidence of intralesional calcification; (B) sagittal CT sinuses (bone algorithm) demonstrating a large polypoidal type opacification obstructing the posterior nasal choanae.
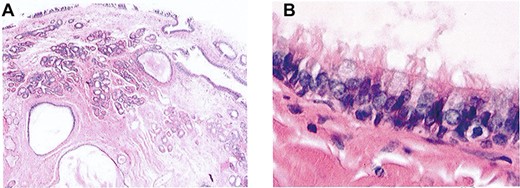
(A) Haematoxylin and eosin staining of lesion demonstrating cystic and glandular structures within a fibrous stroma (light microscopy, ×4); (B) haematoxylin and eosin staining of lesion demonstrating cysts lined by ciliated respiratory type epithelium (light microscopy, ×40).
During clinical and radiological assessment, REAH can masquerade as sinonasal carcinoma [2]. Surgical intervention and adjuvant therapies for sinonasal carcinoma (i.e. squamous cell, adenocarcinoma, adenoid cystic carcinoma, mucosal melanoma) are associated with significant morbidity [1, 2]; consequently, accurate histopathological assessment of REAH is important [4].
CASE REPORT
A 68-year-old gentleman presented with a 2-year history of progressive left nasal obstruction. There was no associated dysgeusia or hyposomnia or anosmia. He was a lifelong non-smoker and was not known to have allergies to medications or an atopic type of rhinosinusitis. He did not have any other significant medical or surgical history and no genetic history of nasal pathologies.
On examination, he had severely reduced left nasal airflow. Anterior rhinoscopy revealed a large fleshy tumour in the left nasal cavity, which was not papillomatous or vascular (Fig. 1). Nasendoscopic examination showed a large tumour of solid and polypoidal components. It occluded the posterior nasal choanae, filling the inferior aspect of the nose. Visualized from the right nostril, the tumour prolapsed into the postnasal space. There was no contact bleeding. The right nasal passage appeared normal. The nasopharyngeal vault and the remainder of the upper airway appeared normal. He did not have otitis media with effusion in the left ear and there was no palpable cervical lymphadenopathy. Pre-operative imaging was ordered to determine the extent of the lesion (Fig. 2).
Treatment was local excision under general anaesthetic. The tumour was attached to the lateral wall of the nose at the level of the middle turbinate and was removed in its entirety excision. There was minimal bleeding and the nasal passage looked otherwise normal. Middle meatal antrostomy revealed scant mucus in the antrum, but the mucosa appeared normal. The perioperative course was uneventful, and the patient was discharged home on the same day.
Histopathology
Macroscopic
The resected mass was a grey polypoidal tissue with spicules of bone measuring 36 × 33 × 18 mm.
Microscopic
Histological examination revealed the mass was lined with ciliated respiratory epithelium, which invaginated into the core of the polyp, forming glandular and cystic structures. There was focal calcification within the cysts. There was a component of bland sero-mucinous glands in lobular arrangements. The epithelial elements were encased in a hyalinized fibrous stroma. No features of atypia or malignancy were visualized (Fig. 3).
Follow up
On follow up, he was asymptomatic and had normal nasal airflow, taste and smell.
DISCUSSION
REAH is a sinonasal tumour characterized by glandular proliferation of the surface epithelium of the nasal cavity and paranasal sinuses [6]. Weinig and Heffner [4] first described it in an analysis of 31 cases.
REAH has the capacity to masquerade as malignancy; consequently, diagnosis is imperative to inhibit aggressive therapy. It is an important differential diagnosis because it can present similarly to other sinonasal lesions, such as inflammatory polyps, inverted papilloma, well-differentiated adenocarcinoma, squamous cell carcinoma, olfactory neuroblastoma and lymphomas [2, 5]. If REAH is misidentified as a more sinister lesion, it can result in over aggressive and/or deforming treatment for a patient [4].
This condition is most common in males aged 30–90 years [1]. Patients present with non-specific symptoms, such as nasal obstruction, epistaxis, hyposomia, chronic sinusitis, deviated septum and frontal headache [5].
Previous reports have identified REAH arising from the nasal septum (especially the posterior aspect); however, we describe the first case arising from the posterior nasal wall [4, 5, 7].
REAH is a complex diagnosis that often cannot be based on clinical findings or radiological evidence alone. REAH most commonly presents as either as a solitary lesion or in association with nasal polyposis, the latter being far more common [3].
Radiologically, the most common finding on a non-contrast-enhanced computed tomography (CT) sinus (bone algorithm) is opacification of sinuses whose ostea are blocked by a posterior nasal cavity polypoid lesion (namely, sphenoid and posterior ethmoid air cells) [1]. Vira et al. [8] retrospectively reviewed the perioperative CT scans of 35 patients with REAH and concluded that there were no distinguishing features that could differentiate it from any other sinonasal lesion. However, a later study found that a widened olfactory cleft, greater than 10 mm on CT imaging, is a characteristic feature of REAH [9]. The olfactory cleft is the distance between the both turbinal ethmoid walls and were significantly increased in patients with REAH in axial (12.2 mm) and coronal (12.1 mm) planes, when compared with patients with nasal polyposis (5.6 and 5.4 mm) and patients with no disease (4.5 and 4.2 mm) [10].
Ultimately, a diagnosis of REAH requires histopathological confirmation in order to definitively differentiate it from other lesions.
Grossly, REAH has a polypoid appearance, with fleshy or firm, yellow–white masses of various sizes [1].
Rom et al. [6] analysed the histopathology of nine samples and found that the tissue showed prominent glandular proliferation, with small- to medium-sized round to oval glands that are widely separated by stromal tissues. These glands are lined by multilayered ciliated respiratory epithelium with goblet cells and have a thick, eosinophilic basement membrane [2]. They do not present with atypia or metaplastic change [8].
With correct identification of REAH, it can be treated with simple excision, compared with sinister sinonasal lesions, which may require aggressive surgical debridement and adjuvant therapies [1]. With appropriate excision, recurrence is extremely rare [7].
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



