-
PDF
- Split View
-
Views
-
Cite
Cite
Romeo Haoudou, Jacques Malghem, Christine Galant, Pierre-Louis Docquier, Painless osteoid osteoma of the distal phalanx of a toe, Journal of Surgical Case Reports, Volume 2021, Issue 2, February 2021, rjaa614, https://doi.org/10.1093/jscr/rjaa614
Close - Share Icon Share
Abstract
Osteoid osteoma is a benign bone tumor, found in young subjects with typical intense focal pain, nocturnal exacerbation and favorable response to salicylates. Painless osteoid osteomas are rare and their diagnosis is difficult, especially whether their imaging appearance is not typical. We report the case of a 13-year-old boy with a spontaneous painless lesion of the distal phalanx of a toe. The main symptom was a swelling of the distal portion of the toe with an enlargement of its nail. The radiological aspect was not typical. A computed tomography showed a small lucent bone area within a focal hypertrophy of the phalangeal tuft and an osteoid osteoma was proposed as main diagnosis. The tumor was completely removed and the histopathological examination confirmed the diagnosis of osteoid osteoma. This clinical case shows that painless swelling of a toe may be indicative of an osteoid osteoma.
INTRODUCTION
Osteoid osteoma represents 2–3% of all bone tumors and 11–14% of benign bone tumors [1]. It mostly affects young subjects, mainly between 5 and 25 year. All bones can be affected, but the most common sites are femur and tibia (50% or more). Ribs, pelvis, patella, metatarsals or phalanges are rare locations [2]. Almost invariably, the main symptom is pain, initially mild and inconstant, and later becoming more severe and persistent with nocturnal exacerbation. A favorable response to salicylates is characteristic of the disease. The radiological diagnosis is based on the demonstration of the lesion, which appears as a regular spherical or elliptical radiolucent area, the nidus, whose diameter is generally <10 mm, with calcification of the central area. It is often poorly visible on radiographs, but it can be identified on computed tomography (CT), and is usually accompanied by adjacent bone sclerosis [2]. This diagnosis can be even more difficult, especially at the extremities, where the very small size of the lesion complicates the radiological analysis. We report a case of osteoid osteoma of the distal phalanx of a toe, which was painless and atypical for its imaging appearance.
CASE REPORT
A 13-year-old male patient presented with swelling of the tip of the third left toe without spontaneous pain. There was acute pain only when pressing on his toe or when shock during sports activities (basketball). Clinically, there was a soft tissue swelling of the distal part of the toe with enlargement of its nail (Fig. 1).

Enlargement of the distal phalanx of the third left toe and its nail.
Conventional radiography showed a discrete deformation and irregular density of the phalangeal tuft (Fig. 2). The color Doppler ultrasound showed a hypervascularized pattern of swollen soft tissues on the dorsal aspect of the phalangeal tuft, suggesting a glomus tumor (Fig. 3). A CT scan showed a small lucent bone area within a focal hypertrophy of the phalangeal tuft with adjacent bone sclerosis (Fig. 4). Based on this latest examination, the diagnosis of OO of the distal phalanx was proposed as diagnosis.
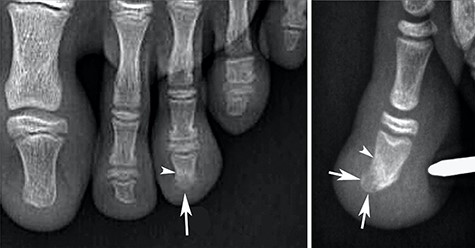
Radiographs showing heterogenous density of the distal phalange of the third toe on the anteroposterior view (arrow in A) and a hypertrophy with low density of the dorsal part of this phalangeal tuft on the lateral view (arrows in B). Note also a discrete densification of the adjacent bone (arrowheads).
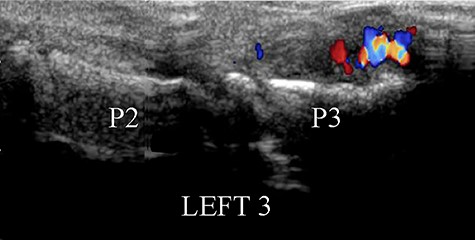
Dorsal view of color Doppler ultrasound showing the hypertrophy of the soft tissues near the phalangeal tuft, with a pattern of hypervascularization.

CT reconstruction images showing a small central lucent bone area in the phalangeal tuft on the coronal plane (arrow in A) and a focal dorsal prominence of the tuft with lucent content (arrow) on the sagittal view (B). Note also the sclerosis of adjacent bone (arrowheads).
An en-bloc resection of the dorsal part of the phalangeal tuft was performed (Fig. 5). The histological examination described a nodule measuring 3 × 2mm, containing an immature osteoid matrix, bordered by osteoclast with many prominent vessels, and surrounded by peripheral osteosclerosis (Fig. 6). This image evoked a nidus and confirmed the diagnosis of OO. The wound healed uneventfully. The pain at the pressure disappeared completely after the operation and no recurrence was observed after 1 year.

(A and B): peroperative views. The nail was removed and the dorsal part of the phalanx tuft was en-bloc resected (A). The nail was reinserted and sutured (B).
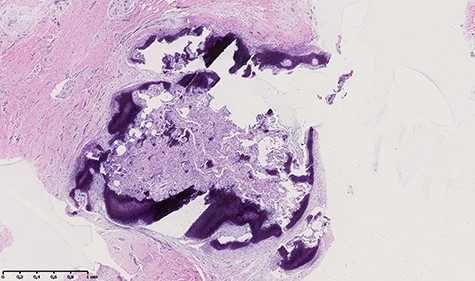
Histologic appearance showing a nodule measuring 3 × 2 mm, containing an immature osteoid matrix, bordered by osteoclast with many prominent vessels, and surrounded by peripheral osteosclerosis.
DISCUSSION
The OO symptomatology is almost always dominated by characteristic pain. However, painless OOs have been reported [3]. Large series cite prevalence of around 2% for painless OOs [2, 4]. The reason for the absence of pain in some OOs is unclear [5]. Hypotheses already formulated such as the periosteal location (lesion decompression by absence of a rigid shell) [6], absence of nerve fibers [7, 8], or locations without axial pressure of body weight [9], have not been confirmed. Painless OOs may be detected by chance or due to thickening of bone or soft tissue when the lesion is close to the skin surface. That explains why OOs of the phalanges account for nearly half of painless OO cases [3]. Painless swelling may also precede the appearance of pain by several years in case of OO located near the surface of the skin [10]. In cases of painless OOs with a deeply location, a functional symptom may be the presenting complaint, for example scoliosis for the spine or a limp for hip.
Actually, pain is not the only clinical sign of OO because, even in painful cases, it is frequently associated with other signs such as swelling of the surrounding soft tissues, or limping if the tumor is located in the lower limbs. Depending on the location, the call symptom may vary.
Most of painless OOs of phalanx reported so far have a similar circumstance of discovery: painless swelling of the finger or toe accompanied by an enlargement of the nail (hippocratism) [7, 10]. Closer the lesion is to the skin, more the inflammation of the surrounding soft tissues will be visible and will manifest itself by swelling, which will not be the case for a deep site (femoral neck for example).
If the radiological appearance of OO is typical, the diagnosis is confirmed easily. The nidus is typically presented in the form of a small radiolucent zone, with sclerosis of surrounding bone which can extend at distance, and with calcification of the central area in the form of radio-opaque spot. For small tumors, central calcification may be lacking, perhaps because the lesion has not yet reached its maturation stage.
A diagnosis of glomus tumor was first considered in our case, because of the hypervascularized pattern in color Doppler ultrasound, and because of the pain that was caused only by compression or shocks against the lesion area. The glomus tumor is known to cause cortical erosion, but it is rare in children. In addition, the glomus tumor can be located against the bone but not within the bone, whereas in our case the radiolucent area was located inside a bony prominence of the phalangeal tuft, as shown in the Fig. 4. At the extremities (hand and foot), in a context of painless local digital swelling with inconclusive imaging, many other differential diagnoses are soft tissue tumors (malignant melanoma, mucoid cyst, epidermoid cyst, tenosynovial giant cell tumor, arteriovenous malformation …), other bone tumors (enchondroma, subungual Dupuytren’s exostosis …), and various other pathologies (inflammatory or microcrystalline diseases, infection, foreign body …).
In the case of our patient, the symptomatology was atypical, and the interpretation of the imagery difficult. En-bloc resection was the best treatment because it served both as an effective diagnostic and therapeutic method without the risk of recurrence. Some authors have suggested that surgical resection should be used as the primary treatment for this type of patient [9].
In conclusion, a diagnosis of OO should be suspected in case of painless swelling or enlargement of a toe or finger.



