-
PDF
- Split View
-
Views
-
Cite
Cite
Cassandra Krause, Michael Chang, Jennifer Veltman, Xian Luo-Owen, Esther Kim, Olumide Danisa, Ahmed M Abou-Zamzam, Kaushik Mukherjee, Lumbar and sacral brucellosis due to queso fresco ingestion, Journal of Surgical Case Reports, Volume 2021, Issue 2, February 2021, rjaa577, https://doi.org/10.1093/jscr/rjaa577
Close - Share Icon Share
Abstract
Brucellosis is rare in the USA, with 100–200 cases reported annually. In this case we illustrate the complex management of spinal brucellosis. A 22-year-old male presented with 3 months of low back pain. Imaging revealed osteomyelitis/diskitis of L5/S1 and abscesses involving the pre-vertebral, epidural and pelvic recesses. Initial biopsies were inconclusive, but the patient later endorsed eating unpasteurized cheese (queso fresco) from Mexico; therefore, Brucella serology was sent and was positive. Despite aggressive antibiotic therapy there was disease progression. The patient underwent debridement of the involved vertebrae and drainage. Multiple cultures failed to grow the organisms, but Brucella polymerase chain reaction was positive. A month later he underwent a second vertebral debridement as well as placement of tobramycin impregnated beads in the vertebral space. He has since recovered. Surgery should be considered if there is a poor response to medical management and patients may need repeated debridement.
INTRODUCTION
Brucellosis is an endemic zoonotic disease and is the cause of up to ~500 000 cases globally; however, it is rare in the USA, with only ~100–200 cases reported each year [1]. The most common mode of transmission to humans has been found to be in unpasteurized dairy products [2, 3].
CASE REPORT
The patient is a 22-year-old previously healthy male who presented to the Emergency Room with a 3-month history of lower back pain elicited after lifting weights at the gym. He also reported intermittent fevers and chills as well as a 20-pound weight loss. He had no recent travel history, worked as a correctional officer and initially denied contact with animals, or consumption of unpasteurized dairy products. On physical exam he had normal vital signs, no spinal or paraspinal tenderness, and no neurologic deficits. A magnetic resonance imaging (MRI) study was notable for findings concerning for discitis/osteomyelitis of L5/S1 with abscess formation (Fig. 1A–C). The patient was admitted and subsequent interventional radiology (IR)-guided biopsies were performed twice, and cultures and pathology were negative for bacteria, fungi and acid-fast bacilli. He was discharged on vancomycin, ceftriaxone and doxycycline for the treatment of osteomyelitis of unknown origin.
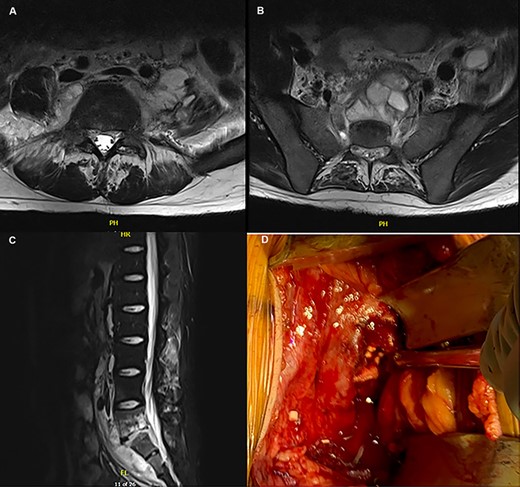
(A–C) MRI depicting the osteomyelitis, discitis and abscess involvement around L5/S1; (D) intraoperative picture of the L5/S1 disc space with placement of tobramycin antibiotic beads.
On follow-up it was discovered that he regularly consumed fresh cheese from Mexico (queso fresco). He had remained symptomatic with fevers. A Brucella antibody was sent and returned positive, therefore gentamicin was added and vancomycin discontinued. A repeat computed tomography scan obtained 4 weeks after the initial MRI showed progression of his infection. The patient was re-admitted to the hospital with spine and acute care surgeons consulted for surgical debridement. Using a left-sided anterior approach (Gibson incision), the retroperitoneum was entered. A large abscess cavity was noted from the L4-S1 pre-vertebral region, continuous with the psoas muscle. This was drained and debrided. He recovered from surgery but developed tinnitus with gentamicin; this was discontinued and the patient was discharged with a 6-week course of ceftriaxone, doxycycline and rifampin.
After 6 weeks of therapy, imaging showed progression of L5-S1 discitis/osteomyelitis and multiple abscess formations. He was admitted for a repeat incision and drainage through an anterior retroperitoneal approach with vascular, spine and acute care surgery. A large abscess was noted anterior to L5/S1, with the infection extending into the disc space. After drainage of the abscess and debridement, tobramycin antibiotic impregnated beads were placed in the disc space (Fig. 1D).
The patient was noted to have initial improvement in his symptoms, but his fevers returned a few days later and another set of imaging studies demonstrated a paravertebral fluid collection. He underwent a drain placement by IR. Following this, he defervesced and was discharged on doxycycline and rifampin treatment for 1 year. Of note, all cultures obtained failed to grow Brucella species, which was only detected on ribosomal polymerase chain reaction (PCR) and serology.
The patient has since returned to full activities and work without any further infectious episodes. The patient provided written consent for publication and use of photographs.
DISCUSSION
Spinal involvement from Brucella is one of the most common complications that can occur from infection with this bacterium [4]. Antimicrobial therapy is the first line treatment for brucellosis infection. Despite appropriate antimicrobial therapy, ~30% of patients may require surgical involvement [5]. Indications for surgical involvement include failure of conservative therapy or onset of neurologic symptoms such as spinal cord compression, weakness or cauda equina syndrome [4]. The presence of abscesses does not mandate surgical treatment or even drainage as there is evidence that antimicrobial treatment may be sufficient to eradicate the organism [4]. In our case, despite appropriate antibiotic treatment for 4 weeks there was no subjective or objective improvement in his infection. His imaging also showed progression of the disease, suggesting an aggressive infection requiring surgical intervention for better source control.
Brucella species additionally have a surface lipopolysaccharide that decreases the ability to mount an adaptive immune response [6]. Furthermore, there is a high risk of relapse, reported to be ~17% [7]. This could be one explanation as to why our patient had to undergo multiple debridements and drainage. A second explanation, though less likely is due to potential partial resistance. There is some evidence that Brucella melitensisis, one of the more common species of Brucella to infect humans, has antimicrobial resistance [8]. Due to the fact that Brucella was never able to be cultured by blood, biopsies or intraoperatively we are unable to determine if resistance did play a role in this case or determine which species of Brucella infected our patient.
There are multiple combinations of antibiotics that can be used for Brucella, with none shown to be superior. The different combinations include: doxycycline, ciprofloxacin and rifampin; an aminoglycoside such as gentamicin or streptomycin with rifampin and doxycycline; doxycycline and rifampin; trimetroprim-sulfamethaxole (TMP-SMX) combined with an aminoglycoside; and ceftriaxone with TMP-SMX and rifampin [9]. Most of the regimens do include an aminoglycoside; however, due to the adverse reaction that our patient had gentamycin was discontinued and he was continued on doxycycline and rifampin, which has not been shown to be inferior in effectiveness [9].
It is important for clinicians to be aware of this disease and keep it in their differential diagnosis for patients with unexplained fevers in conjunction with musculoskeletal symptoms. Although rare in the USA, brucellosis is endemic in regions close to the USA, such as Mexico [1]. When this disease is suspected, the recommendation is to obtain blood cultures and potentially bone marrow cultures, however if this is negative, as it was in our patient, a suitable alternative is PCR [10].
A multi-disciplinary approach is needed to manage a complex spinal brucellosis infection. Initial management should consist of aggressive and prolonged antibiotic therapy. Surgery should be considered if there is a poor response to medical management.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
- polymerase chain reaction
- biopsy
- brucellosis
- debridement
- abscess
- brucella
- cheese
- discitis
- disease progression
- low back pain
- mexico
- osteomyelitis
- serologic tests
- surgical procedures, operative
- diagnostic imaging
- eating
- pelvis
- study of serum
- tobramycin
- antibiotic therapy
- ingestion
- vertebrae
- medical management



