-
PDF
- Split View
-
Views
-
Cite
Cite
Megan Jenkins Turner, Lutfi Barghuthi, Tyler Davis, Hishaam Ismael, Traumatic rupture of a hemorrhagic hepatic cyst: a case presentation and literature review, Journal of Surgical Case Reports, Volume 2021, Issue 12, December 2021, rjab545, https://doi.org/10.1093/jscr/rjab545
Close - Share Icon Share
Abstract
Hemorrhagic hepatic cyst with or without rupture is rare cause of acute abdomen with less than 20 cases reported in the literature. A standardardized management algorithm is currently not present, but literature suggests surgical management is ideal for definitive treatment and successful patient outcome. We report a case of a 39-year-old female with a chief complaint of sudden onset abdominal pain, nausea and vomiting. Abdominal computed tomography scan showed a large, 12-cm cyst in the right hepatic lobe with a hemorrhagic component. Successful laparoscopic operative management was conducted without post-operative complications such as recurrent bleeding. When managing patients with an acute abdomen, ruptured hepatic hemorrhagic cysts should be considered in the differential diagnosis and prompt surgical management should be considered as primary management.
INTRODUCTION
Simple cysts of the liver are common and found in 1% of the population. On the other hand, hemorrhagic hepatic cysts are found in 1–5% of the population, are more common in women (3:1) >60 years old, and are most commonly asymptomatic [1, 2].
Hemorrhagic rupture of hepatic cysts is rare, but can be life threatening if surgical intervention is not prioritized [3, 4]. Although rare, sudden and persistent hemorrhage occurs in up to nearly 40% of cases reported, whereas severe abdominal pain is the most common symptom on presentation (> 90% of patients) [1–12]. A standard management algorithm for ruptured hepatic cysts is currently not formally described, but literature suggests surgical management is ideal for treatment to eliminate recurrent hemorrhage and abdominal pain [3].
CASE REPORT
We present a case of a 39-year-old Hispanic female who presented through the emergency department (ED) with severe right upper quadrant stabbing pain radiating to her back. The pain started several weeks prior and steadily progressed to include nausea and vomiting over the past few days. The patient reported that her pain progressively worsened over time after ‘massaging her right side’ regularly. Her past medical history included hypertension, diabetes mellitus Type II, hyperlipidemia and endometriosis. She denied illicit drug and tobacco use and admitted to drinking alcohol socially. Home medications included: Insulin, Lisinopril, Lovastatin, Metformin and Norethindrone. Her surgical history was pertinent for right oophorectomy and subsequent hysterectomy with left salpingoophorectomy due to complications of endometriosis.
Her vital signs on admission were 167/99 mm Hg, 90 bmp, 18 breaths/min and 99.1°F. Her physical examination was remarkable for focal right upper quadrant tenderness to soft palpation. Her hemoglobin was 12.1 g/dl (14–18 g/dl), HCT 37.9 g/dl (38–54 g/dl), WBC count 10.08 g/dl (3.8–10.6 g/dl), AST 60 u/l (0–37 u/l) and ALT 86 u/l (12–78 u/l).
A computed tomography (CT) scan with intravenous (IV) contrast of the abdomen (Fig. 1) was performed and demonstrated a large 12 × 11 × 10 cm round exophytic complex hepatic cyst containing central soft tissue density mass and septations with multiple small hepatic cysts throughout liver. A hemorrhagic component within the cyst was also seen. In order to further delineate the cyst’s relationship to the biliary tree and surrounding structures, magnetic resonance imaging (Fig. 2) was also performed and a large exophytic peripherally cystic lesion with central solid non-enhancing component in inferior right lobe of the liver was seen. There was no evidence to suggest free rupture, communication to the biliary tree or hemobilia. The patient was admitted for close monitoring and on the third day her abdominal examination progressed to include tenderness in all quadrants of the abdomen with peritoneal signs. The patient received two packed red blood cell transfusions due to a drop in hemoglobin (12.1–8.8 g/dl) associated with tachycardia up to 131 bpm. Surgical management was discussed with the patient and she agreed to proceed.
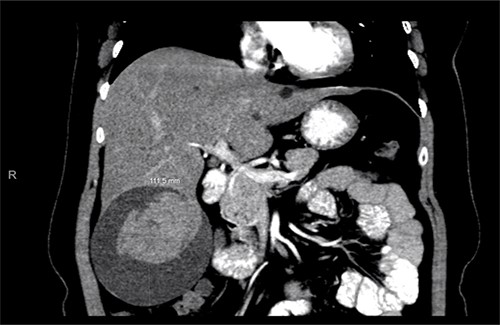
Abdominal CT scan showing a large cyst 12 × 11 × 10 cm in the right hepatic lobe with a hemorrhagic component.
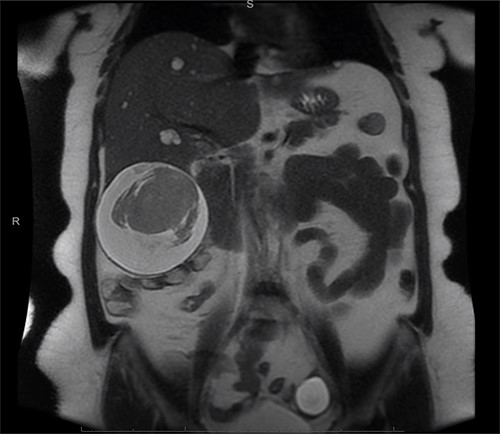
Exophytic peripheral cystic lesion with central solid non-enhancing component in inferior right lobe of the liver.
Diagnostic laparoscopy revealed a large ruptured, segment six, liver cyst with ~500 ml of blood suctioned from the abdomen. The majority of the liver cyst was exophytic. A harmonic (ultrasound energy device) was used to perform a partial hepatectomy (deroofing). The majority of the cyst wall was removed leaving minimal cyst wall at the liver bed (Fig. 3). Histopathology report detailed fragments of benign simple cyst wall and blood clot, without any evidence of malignancy. The patient had no post-operative complications and was sent home on post-operative day two. She was seen at her 2-week and 3-month post-operative clinic follow up. She had an uneventful recovery from her operation.
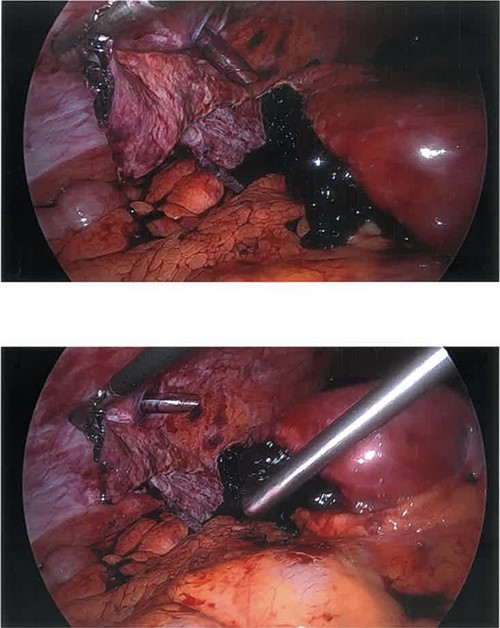
Ruptured hemorrhagic hepatic cyst wall and remaining hemorrhagic component mid-suctioning.
DISCUSSION
Standard methods of management for ruptured hepatic cysts are currently not formally described in the literature, but surgical management is clearly the definitive treatment quenching the likelihood of recurrent hemorrhage, progression of anemia and worsening abdominal pain [3]. Percutaneous drainage may be considered when managing hepatic hemorrhagic cysts. However, the recurrence rate of the cyst is >80% and is associated with further hemorrhage and subsequently the likelihood of acute abdomen and the need for emergent surgery [3]. It is also important to note that >50% of patients with hemorrhagic liver cysts present to the ED after a traumatic inciting event such as: massaging the cyst (our patient), pregnancy and recent abdominal contusion and/or ground level fall [1, 3, 5–7].
The majority (61.5%) of cases reported in the literature were treated using a laparoscopic deroofing and washout approach with or without partial hepatectomy. In 38.5% of cases, however, emergent laparotomy was performed due to hemodynamic instability on presentation. All 12 cases reviewed in the literature reportedly resulted in no post-operative complications or sequala with patients discharged between post-operative Days 2–10 [1–12]. Although the data are limited on non-surgical management of hemorrhagic liver cysts, it can be concluded that surgical management is ideal especially when considering two patient cases who were treated with conservative management on initial presentation. A few months later, both patients went on to develop acute abdomens and continual hemorrhage ultimately receiving laparoscopic operative management with no recurrent bleeding post-operatively [2, 7].
CONCLUSION
Ruptured hemorrhagic liver cysts are rare but should be considered in the differential diagnosis of acute abdomen particularly when hemodynamic instability is present. Surgical management should be deemed the primary treatment modality when a hemorrhagic hepatic cyst is diagnosed so that continued hemorrhage and abdominal pain does not persist putting the patient at risk for blood-loss anemia and hemodynamic instability.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None declared.



