-
PDF
- Split View
-
Views
-
Cite
Cite
Andy Chao Hsuan Lee, Andrew Gorton, Andy Tully, ShouJin Wu, Francis J Podbielski, Surgical management of locally invasive basaloid carcinoma of thymic gland, Journal of Surgical Case Reports, Volume 2021, Issue 11, November 2021, rjab531, https://doi.org/10.1093/jscr/rjab531
Close - Share Icon Share
Abstract
Thymic basaloid carcinoma is an extremely rare thymic tumor variant, and the most common presentations have been an incidental finding on a routine chest X-ray and dyspnea on exertion. Given its rarity, no treatment modalities have been demonstrated to improve survival. This rare case describes a patient with locally advanced thymic basaloid carcinoma treated by en bloc resection of phrenic nerve and left upper lobe with the tumor followed by adjuvant radiation therapy. Patient had no respiratory complaints at 10 months follow-up, and 10-month post-operative surveillance radiological study showed no objective sign of tumor recurrence.
INTRODUCTION
Thymic basaloid carcinoma is a rare thymic tumor variant that only a few cases have been reported in the literature [1]. In previous studies, evaluation of various treatment modalities used to treat patients with all types of thymic carcinomas did not yield any statistically significant correlations with survival [2, 3]. We herein present a case of locally advanced thymic basaloid carcinoma treated by aggressive surgical management with en bloc resection of surrounding structures followed by adjuvant radiation therapy.
CASE REPORT
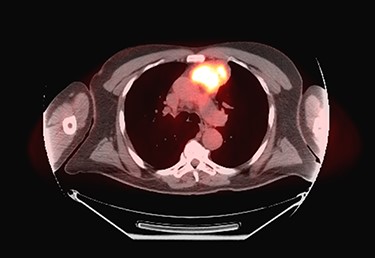
Sixty-three-year-old male was with the history of diabetes and hypertension who presented with 2 days of new onset, intermittent and non-pleuritic left-sided chest pain, with a few months of new onset exertional dyspnea. Chest X-ray showed a convex shaped mass at the left hilum. Chest CT angiography revealed a 5.6 × 7.1 × 5.4 cm hypodense mass in the anterior mediastinum involving the adjacent anterior medial left upper lobe, and adjacent mildly enlarged aorticopulmonary window lymph nodes (Fig. 1). PET scan demonstrated a hypermetabolic anterior mediastinal mass adjacent to medial left upper lobe highly suggestive of malignancy (Fig. 2). Ultrasound-guided core needle biopsy showed nests of small cells with peripheral palisading and focal abrupt transition to squamous cell, consistent with basaloid carcinoma of thymic gland. Immunostainings of the tumor cells were positive for cytokeratin AE1/AE3, cytokeratin CK904, p63 and p40.

Chest CT angiography revealed a 5.6 × 7.1 × 5.4 cm hypodense mass in the anterior mediastinum involving the adjacent anterior medial left upper lobe.
Pre-operative PET scan demonstrating a hypermetabolic anterior mediastinal mass.
Patient underwent resection of the mediastinal mass. A median sternotomy was performed in typical fashion. Dissection was carried out along the innominate vein where significant desmoplastic reaction from the tumor was present. Upon entry into left chest, the tumor was noted to have contiguous spread into the left upper lobe that unfortunately involved a substantial portion of the phrenic nerve. Decision was made to divide the left phrenic nerve and resect a wedge of left upper lobe en bloc with the tumor. Final pathology report described a 10.2 × 7.5 × 6.0 cm tumor with histology consistent with basaloid carcinoma of thymic gland, with involvement of pulmonary parenchyma and presence of lympho-vascular invasion (Fig. 3). All margins were negative with closest margin being 3 mm. Final pathological stage was pT3N0M0.
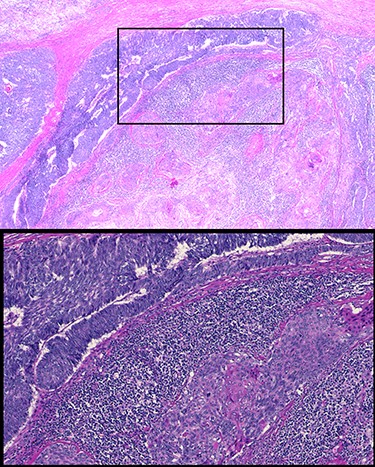
Histology of resected thymic gland with enlarged inset showing palisading and squamous features highly suggestive of basaloid carcinoma.
Patient’s post-operative course was notable for prolonged respiratory support due to phrenic nerve deficit. Patient’s respiratory failure resolved with 5-day course of intravenous antibiotics, spot diuresis and respiratory therapy. Patient was discharged home on post-operative day 10 day. Patient completed adjuvant radiation therapy at a total dose of 50 Gy in 25 fractions to the post-operative bed and anterior mediastinum. At 10-month follow-up, patient had no respiratory complaints with surveillance PET study showing no objective sign of tumor recurrence (Fig. 4).
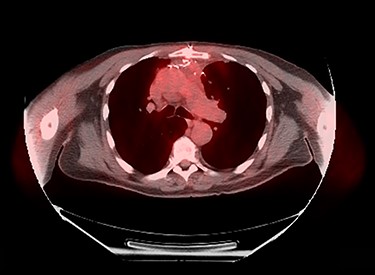
Ten-month post-operative surveillance PET scan demonstrating no evidence of tumor recurrence.
DISCUSSION
Primary thymic carcinoma is a rare malignancy and particularly basaloid type is an even rarer subtype, with less than 20 cases published as individual case reports in the English literature [4]. According to literature, the most common presentations have been an incidental finding on a routine chest X-ray and dyspnea on exertion, while two cases reported chest pain on initial presentation [5]. Morphologically, basaloid carcinoma of thymic gland exhibits peripheral palisading and pseudoglandular formations and is often associated with a squamous component. Immunohistochemically, thymic basaloid carcinoma is positive for cytokeratin [5], which was demonstrated in our case.
Our patient had at presentation a locally advanced tumor with pulmonary and phrenic nerve involvement but no clear evidence of extra-thoracic spread or involvement of other mediastinal structures. Given rarity of primary thymic basaloid carcinoma, the clinical benefits of any treatment modality remain unclear [2, 3]. In almost all previously published cases, surgical excision has been the recommended treatment and has been performed in almost all cases [3]. In our case, we extrapolated the treatment for thymic basaloid carcinoma from that for thymic carcinoma, an aggressive tumor with poorer prognosis and higher mortality than thymomas [6]. Previous study has suggested that the extent of surgical resection was critical given that incomplete resection was a strong independent predictor of progression-free survival in thymic carcinoma [6]. Thus, we were aggressive in performing the resection by taking a wedge of left upper lobe and a segment of left phrenic nerve en bloc with the tumor.
This case describes a patient with a rare case of locally advanced thymic basaloid carcinoma successfully treated by en-bloc resection of the tumor with phrenic nerve and left upper lobe followed by adjuvant radiation therapy. Given no treatment modalities have been demonstrated to improve survival in literature, the present case may suggest the efficacy and safety of extended resection of tumor followed by radiation therapy in treating this rare disease.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



