-
PDF
- Split View
-
Views
-
Cite
Cite
Abdoul Kader Tapsoba, Moez Rahoui, Mokhtar Bibi, Beya Chelly, Yassine Ouanes, Kays Chaker, Kheireddine Mrad Dali, Ahmed Sellami, Sami Ben Rhouma, Yassine Nouira, An unusual association of adenocarcinoma and isolated tuberculosis of prostate gland, Journal of Surgical Case Reports, Volume 2021, Issue 11, November 2021, rjab504, https://doi.org/10.1093/jscr/rjab504
Close - Share Icon Share
Abstract
Adenocarcinoma of prostate is the most common primary prostatic malignancy in the world. Isolated prostate tuberculosis is an uncommon type of tuberculosis. Concomitant occurrence of both conditions is extremely rare. We report two cases of adenocarcinoma and tuberculosis of the prostate. The patients were 83 and 74 years old, respectively. They presented obstructive and irritative symptoms of the lower urinary tract. The prostatic finding and prostate-specific antigen were abnormals. The diagnosis of prostatic tuberculosis and adenocarcinoma was made by histologic analysis after transurethral resection of prostate. The treatment is based on chemotherapy anti-tuberculosis and hormonotherapy. Tuberculosis and malignancy may co-exist in some cases and clinicians must have a high index of suspicion for tuberculosis, especially in patients from endemic areas, in order to initiate early and proper treatment.
INTRODUCTION
Tuberculosis (TB) is a major health problem in Tunisia. According to World Health Organization, TB incidence, in 2019, was 35 cases/100 000 population in Tunisia [1]. Urogenital tuberculosis (UGTB) represented 30–40% of all extrapulmonary cases [2]. Among the urogenital organs, prostatic TB is less common. The concomitant presence of TB and adenocarcinoma in prostate gland is extremely rare. We report two cases of unusual presentation of tuberculous and prostate cancer in immunocompetent patients.
CASE REPORTS
Case 1
An 83-year-old man consulted for an obstructive lower urinary tract symptoms (LUTS) involving urinary frequency and dysuria lasting. The patient underwent transurethral resection of the prostate (TURP) in 2006 and 2017, after failure of well conducted medical treatment (alpha lytics and 5 alpha reductase inhibitor) of symptomatic benign prostatic hyperplasia. No history of pulmonary TB was noted. The patient was vaccinated with BCG in childhood and he had no family history of TB. Digital rectal examination showed an enlarged prostate with hard consistency and nodular surface. Biology found an elevation rate of prostate specific antigen (PSA 78 ng/ml). The urine culture was sterile. HIV serology was negative. The prostate ultrasound showed a heterogeneous prostate, enlarged, whose weight was estimated at 65 g and post-void residual volume (PVR) at 150 cc. The chest X-ray was normal. A prostate cancer was suspected. We performed an echo-guided prostate biopsy, which confirmed the diagnosis of adenocarcinoma of the prostate Gleason 8 (4 + 4), and a TURP was subsequently performed for voiding purposes. The histopathological examinations showed the existence of prostatic adenocarcinoma Gleason 8 (4 + 4) and more follicles with giant cells and Caseous necrosis in favour of an evolutive caseo-follicular tuberculous prostatitis (Fig. 1a and b). We performed an intravenous urographic examination without finding any abnormalities in other structures of the urinary tract. The patient received 6 months of anti-TB treatment. Four antibiotics (rifampicin, isoniazid, pyrazinamide and ethambutol) for 2 months followed by two antibiotics (isoniazid and rifampicin) for 4 months. A hormonal treatment based on triptorelin injection 11.25 mg every 3 months was associated. After 1 year, the outcome was uneventful with improvement of LUTS and a PSA level at 0.22 ng/ml.
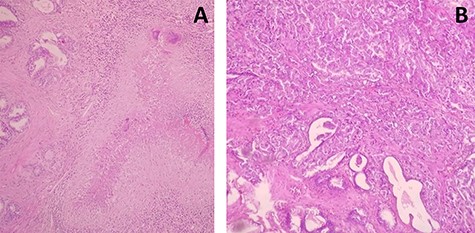
(A) Prostatic parenchyma seat granuloma epithelioid and giant cell centered by a caseous necrosis (haematoxylin and eosin ×40). (B) Carcinomatous proliferations organized in glandular structures realizing cribriform and polyadenoid clusters (haematoxylin and eosin ×100).
Case 2
A 79-year-old man presented with a 4-week history of an obstructive LUTS. He was admitted to the department for acute retention of urine drained by trans-urethral catheter. The digital rectal examination showed an enlarged prostate with a hard consistency and nodular surface. The PSA level was 69 ng/ml. The prostate ultrasound showed a heterogeneous prostate of 65 g with areas of calcification in the centre and PVR at 120 cc. The diagnosis of prostate cancer was strongly suspected. We performed an ultrasound-guided prostate biopsy, and the histopathological findings were adenocarcinoma Gleason 6 (3 + 3). And we had done a TURP for micturition purposes. The histopathological examination was in favour of prostatic TB (caseous necrosis and Langhans giant cell isolated) and adenocarcinoma prostatic Gleason 6 (3 + 3). Intravenous urography and chest radiography are without particularities. The patient received the same treatment regimen like the first case with a 2-year uneventful follow-up, a very good clinical improvement was observed and a PSA of 0.13 ng/ml.
DISCUSSION
Prostate TB, especially isolated, is extremely rare. The first case was described in 1882 by Jasmin. Its incidence is estimated at 6.6% of the UGTB according to Scotch Brady Urological Institute in Baltimore [3].
The association of TB and carcinoma was initially described 200 years ago by Bayle who considered “Cavitation Cancereuse” as one of the various types of TB. Ever since, the potential association between TB and subsequent development of cancer has been investigated [4].
The association between TB and malignancy may be merely incidental, as both conditions are common. However, there is a growing body of evidence suggesting that mycobacterial infection may play a role in carcinogenesis [5]. Mycobacterium TB has been shown to have the ability to induce DNA damage via the production of reactive oxygen species [6]. Moreover, the organism may exhibit increased expression of anti-apoptotic activity [7]. An experimental study has shown that the purified protein derivative of tuberculin can upregulate the expression of vascular endothelial growth factor in lymphocytes, which has significant angiogenic and mitogenic properties [8].
Lastly, it is well known that chronic inflammation, as in mycobacterial infection, is a potential factor in the development of cancers and metastatic spread [9].
The combination of direct DNA damage, apoptosis inhibition and perpetuation of chronic inflammation may enhance mutagenesis of progeny cells and these effects, coupled with enhanced angiogenesis, may lead to a microenvironment that is highly conducive to tumorigenesis [5].
Since both disorders are common, we support the notion that in most cases their co-existence may be explained by chance alone.
CONCLUSION
TB and malignancy may co-exist in some cases and clinicians must have a high index of suspicion for TB, especially in patients from endemic areas, in order to initiate early and proper treatment. Further work is needed to better understand the role of TB in malignancies.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The approval of the current study has been granted by the medical committee of research ethics of La Rabta Hospital. Written informed consent was obtained from the patient for publication of this study. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.
FUNDING
No funding was received.



