-
PDF
- Split View
-
Views
-
Cite
Cite
Abdulaziz K Alaraifi, Danah F Alrusayyis, Abdullah Alzuwayed, Fahad Alobaid, Mohammed AlRajeh, Riyadh Alhedaithy, Endoscopic transorbital management of frontal sinus mucocele: a case report and review of the literature, Journal of Surgical Case Reports, Volume 2021, Issue 10, October 2021, rjab491, https://doi.org/10.1093/jscr/rjab491
Close - Share Icon Share
Abstract
The frontal sinus is the most common site for paranasal mucoceles, resulting in potentially threatening intraorbital or intracranial complications. Surgical drainage of mucoceles is the mainstay of treatment, which can be achieved usually through open or endoscopic transnasal approaches. Transorbital endoscopic surgery is a relatively novel approach to selective skull base lesions with limited data in the literature. It could be utilized as a safe and effective alternative approach in managing frontal sinus lesions when the endoscopic transnasal access alone is insufficient or inadequate. Here, we present a case of an isolated lateral left frontal mucocele that was managed successfully using an endoscopic transorbital approach alone with complete resolution of symptoms during a 10-month follow-up period.
INTRODUCTION
The most common site of sinonasal mucoceles is the frontal sinus, accounting for 60–89% of all sinonasal mucoceles [1]. The transnasal endoscopic approach is considered the gold standard for sinonasal pathologies with only a few limitations [2]. Transorbital endoscopic approach (TOEA) is a novel technique that was described by Moe et al. [3] in 2011 for the management of paranasal sinus and anterior skull base pathologies. External and endoscopic transnasal approaches are well studied in the literature in comparison to TOEA. This case demonstrates the successful management of an isolated frontal mucocele using TOEA alone without complications.
CASE REPORT
A 58-year-old male presented to the emergency department with a left eyelid swelling associated with mild to moderate pain for a 2-week duration. The patient did not have any visual changes, sinonasal symptoms, and neither fever nor constitutional symptoms. The patient’s past history was only significant for left parietal craniotomy due to head trauma 40 years ago.
The left eyelid swelling was causing inferior globe dystopia with mild tenderness on palpation, but no redness, fluctuation or cutaneous changes (Fig. 1). The extraocular muscle movements were intact, except for limited left supraduction due to the eyelid swelling. The pupils were equal and reactive, and visual acuity and color vision were normal. Transnasal endoscopic examination was unremarkable bilaterally. Contrasted sinus computed tomography (CT) scan showed an expanding left frontal sinus hyperdense opacification with peripheral enhancement and extension to the left orbit (Fig. 2). Magnetic resonance imaging (MRI) showed a loculated mucocele in the left frontal sinus with hypertense T1 signal and extension to left orbit but no intracranial extension (Fig. 3).

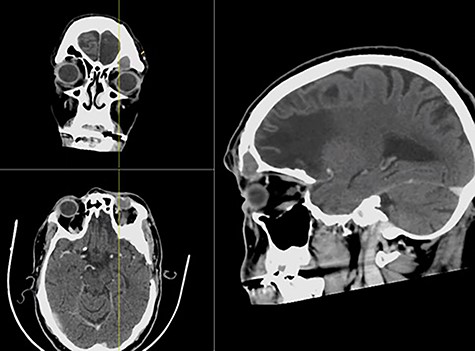
CT with contrast showing a complete left frontal sinus opacification with an inferior bony defect and extension to the left globe and obstruction of the frontal sinus drainage pathway in coronal (a), axial (b) and sagittal (c) views.
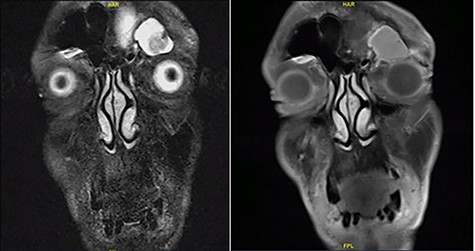
Face MRI showing a mass in the left frontal sinus with hypertense T1 signal and extension to left orbit.
TOEA was selected after consulting the oculoplastic surgeon due to the lateral location of the frontal mucocele in addition to being an isolated mucocele with frontal sinus outflow obstruction. The frontal mucocele was successfully removed using TOEA through superior lid crease (SLC) incision followed by orbicularis oculi dissection, which exposed the orbital septum. The dissection until the superior orbital rim was exposed. The periosteum of the orbital rim was incised and peeled off, which exposed a bulging mass medially. The mass with surrounding fibrosis was excised completely and sent for histopathological evaluation. A bony defect was revealed at the lower aspect of the left frontal sinus measuring around 1.5 × 2.0 cm (Fig. 4). The left frontal sinus cavity was visualized completely through the bony defect using a combination of 0-degree and angled endoscopes. This revealed an isolated frontal sinus cavity with a completely obstructed frontal sinus drainage pathway medially, as a result of the previous head trauma sustained 40 years ago. Then, the frontal sinus mucosa was peeled off entirely from the bone using angled curettes followed by complete obliteration of the frontal sinus cavity using s fat graft harvested from a small incision on the left periumbilical area (Fig. 5). The periosteum of the orbital rim and the skin incision were closed using multiple 5-0 Vicryl and 6-0 Vicryl Rapide sutures, respectively. The patient made an uneventful postoperative recovery and was discharged on the following day of the surgery in a stable condition.

(a, b) Trans-orbital superior lid crease marking of the left eye and dissection until reaching the orbital rim. (c, d) A medial bulging mass was removed leaving a defect at lower aspect of left frontal sinus.
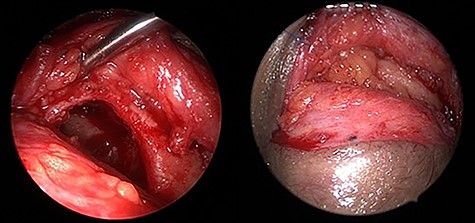
Endoscopic transorbital view of the isolated left frontal sinus cavity after completely peeling off the frontal sinus mucosa (a) and after fat obliteration of the cavity (b).
Histopathology examination showed fibro-adipose tissue with granulation tissue formation, fibrosis and mucoid degeneration, which is consistent with mucocele. The patient was seen in the clinic regularly postoperatively and reported no active complaint with a nicely healed scar and resolved periorbital edema and globe dystopia (Fig. 6).
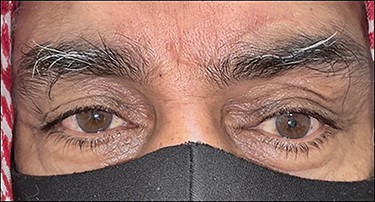
A 3-month-postoperative picture showing improved left globe dystopia and resolved fullness and swelling.
DISCUSSION
The most common complaints of frontal mucoceles are headache and ocular symptoms. Patients may exhibit orbital displacement, proptosis, diplopia, ophthalmoplegia and decreased visual acuity [4, 5]. Paranasal sinus CT scan is the gold standard confirmatory test, which can trace the extent of mucoceles and help navigate through the sinuses [6]. MRI can also be performed if an intracranial or orbital extension is suspected, as in our case [7].
The goal of surgery is to eradicate the mucoceles, ventilate the sinuses, and decrease morbidity and recurrence [8]. Open obliterative procedures were the gold standard in the management of frontal mucoceles until the late 1980s [9]. Since that time, there has been an increase in the use of transnasal endoscopic approach, which is considered the gold standard in the management of sinus pathologies [2, 10]. However, there are a few locations that are anatomically or technically challenging to access using transnasal endoscopic approach alone, such as superior orbit and lateral frontal sinus [11]. Even though adding external approaches, such as frontal trephine, are of proven efficacy and safety profiles, the advancement of TOEA has provided a more favorable path-to-target trajectory and more comprehensive access than previously mentioned approaches [11, 12]. TOEA allows feasible, direct navigation to mucoceles located laterally in the frontal sinus or extended to the anterior cranial fossa [2, 11, 12]. The routes for access vary according to the targeted site and include SLC, pre-caruncular (PC), inferior transconjunctival (ITC) and lateral retro-canthal (LRC) [3].
Special attention to specific steps must be regarded when surgeons choose to adopt SLC approach, such as preserving the supraorbital and supratrochlear neurovascular bundles, and reconstruction of the defect to counteract the prolapse of orbital contents. The reconstruction can be done by using a fat graft, as in our case, or a single sheet of 0.25 mm polydioxanone (PDS) situated between the bone defect and the periosteum [11].
Miller et al. [11] conducted a retrospective case series that included patients who underwent TOEA for sinus mucocele. The most common etiology was isolated craniofacial trauma. Nearly half of the patients had a history of a previous surgical repair, and 24% had a history of failed surgical drainage of mucocele via a non-transorbital approach. Our patient has a positive history of head trauma and open surgery, which constitute the most significant risk factors reported in the literature.
Locatelli et al. [13] have conducted a meta-analysis to investigate TOEA outcomes in treating various extradural and intradural conditions. No reports of postoperative bleeding, surgical site infection, permanent visual impairment or CSF leaks were documented. Only rare cases reported diplopia, palpebral ptosis, epiphora and enophthalmos as postoperative complications. Our patient only had an expected mild postoperative periorbital edema that showed complete resolution after few weeks.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest.
FUNDING
No funding was received for this study.



