-
PDF
- Split View
-
Views
-
Cite
Cite
E Zúñiga-Garza, A Aldape-Mora, D A Chávez-Fernández, J A Rodríguez-Osuna, M Onofre-Borja, R A López-Saucedo, Giant mature cystic teratoma of the mediastinum resected by VATS: a case report, Journal of Surgical Case Reports, Volume 2021, Issue 10, October 2021, rjab474, https://doi.org/10.1093/jscr/rjab474
Close - Share Icon Share
Abstract
The incidence of mediastinal teratomas is low, it’s important to recognize them between all the differential diagnoses for mediastinal tumors. The treatment is surgical resection.
We report a giant mature cystic teratoma of the mediastinum in a 40-year-old woman. She presented with dyspnea, flu-like symptoms during the previous 5 days. An x-ray complemented with a chest CT scan showed a heterogeneous extrapulmonary multiloculated and predominantly fluid density tumor located at the left side of the mediastinum. The patient underwent resection by video-assisted thoracic surgery (VATS). The tumor was 15 cm in diameter with a predominant cystic component. Histologic examination revealed a mature cystic teratoma.
Treatment of these tumors should attempt a complete resection. Open approaches are painful, require a longer recovery and are associated with higher morbidity. VATS has been used to treat these tumors, demonstrating the same effectiveness and advantages over open procedures.
INTRODUCTION
Teratomas are benign or malignant tumors, and they are formed by any of the three germ layers (ectoderm, endoderm or mesoderm). Diagnosis requires the presence of components from two of the three embryological layers, which can include: teeth, epidermis or hair (ectoderm); cartilage or bone (mesoderm), and bronchial, intestinal or pancreatic tissue (endoderm) among others [1]. Mediastinal teratomas are rare, accounting for 5%–10% of all mediastinal tumors [2]. Complete surgical resection is the treatment of choice and multiple approaches can be used such as sternotomy, anterior thoracotomy, posterolateral thoracotomy or minimally invasive techniques. We present a clinical case report of a patient with a giant mature cystic teratoma of the mediastinum successfully treated with VATS [3, 4].
CASE REPORT
A 40-year-old female patient with a history of hypothyroidism was presented to the hospital with 5-day long flu-like symptoms (malaise, rhinorrhea and chills) along with cough and fever. By the time of her admission, she presented with dyspnea and an oxygen saturation level of 85%. On examination, the temperature was 37°C, respiratory rate 24 cycles/min, pulse rate 98 bpm, blood pressure 105/60 mm Hg. Rales were present at both pulmonary bases and mild abdominal pain was found on palpation over the upper right quadrant without peritoneal irritation signs. A chest x-ray was performed showing a radiopaque image at the left side of the cardiac silhouette from the second and seventh costal arc, deviation of the airway to the right side, and absence of pleural effusion (Fig. 1). A CT scan revealed a heterogeneous extrapulmonary multiloculated and predominantly fluid density lesion. It was located at the anterior mediastinum with left lateral extension. On intravenous contrast administration, wall enhancement of the lesion was observed, without pericardium involvement (Fig. 2).
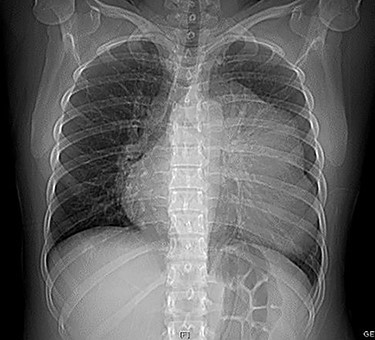
Chest x-ray showing a radiopaque image at the left side of the cardiac silhouette from the second to seventh costal arc and deviation of the airway to the right side without pleural effusion.
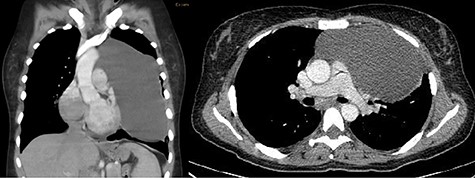
(A) Coronal venous phase tomography showing a heterogeneous extrapulmonary multiloculated and predominantly fluid density tumor located in the left side lateral to the mediastinum with wall enhancement of the borders and no pericardium involvement. (B) Axial delayed phase tomography showing invasion of the tumor to the right thorax.
Before surgery, the cystic tumor was punctured in a separate session with ultrasound-guided technique by a pulmonologist to generate space in the thoracic cavity, obtaining a thick yellowish fluid (Fig. 3). After that, surgical treatment was indicated with a VATS approach. The camera was inserted through a 1 cm incision in the seventh intercostal space (ICS) on the posterior axillary line, a small working incision was made in the fourth ICS between anterior and midaxillary lines for thoracoscopic instruments. Upon entering the left thorax, a 15 cm diameter cystic tumor was observed, the tumor was firmly adherent to the pericardium, contralateral pleura and great vessels. A small part of the lung was resected en bloc together with the cystic tumor, which was removed successfully without intraoperative complications. A 24-French silicon closed drain was left in place.

Yellowish and dense fluid obtained from the tumor by US-guided puncture.
After surgery, the patient developed right lobar atelectasis (Fig. 4), which was treated with respiratory physiotherapy and rehabilitation. She was discharged 8 days after surgery and the drain was removed during the follow-up examination on the 13th postoperative day. Histologic examination showed a mature cystic teratoma without malignant characteristics (Fig. 5). No recurrence was found during a 24-month follow-up.

(A) Immediate postoperative view. (B) Postoperative CT scan showing absence of the tumor and a right lobar atelectasis.
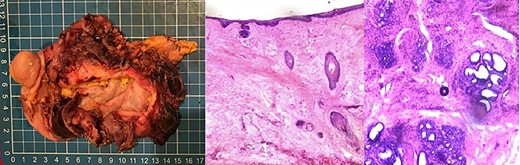
(A) Gross resection specimen. The tumor was predominantly cystic, with a smooth internal lining. Its content was yellowish and pasty, with some hair. The solid component was light brown and rubbery consistency. (B) H & E at 40×. The wall was formed by epidermis and dermis with some hair follicles. (C) H & E 40×. Within the solid component, there were mucosecretory glands with columnar epithelium, serous acini and ducts lined by columnar epithelium. No signs of atypia were observed.
DISCUSSION
Mature mediastinal teratomas are rare entities, representing 5%–10% of all mediastinal tumors [5], which are more frequently found in the anterior mediastinum. They can be benign or malignant and are usually asymptomatic due to their slow growth. Mature and benign forms predominate; however, they have a potential risk of malignant transformation [6]. Most of the series reported do not find a predilection for sex; in a case series carried out by Wychulis, from the Mayo Clinic, a slight predominance of the female sex was found [6]. It occurs at an early age, mostly between 20 and 40 years old [7]. When symptoms are present, the most common is chest pain, usually located at the sternal level or toward a hemithorax in case the tumor protrudes laterally and involves the parietal pleura. They may also present with cough due to compression or irritation of the airway; an unusual but pathognomonic sign is the expectoration of hair follicles, known as trichoptysis.
Histologically they can contain any tissue derived from the three germ layers, but must include at least two of them.
Treatment of these tumors involves complete resection, to distinguish between benign and malignant lesions, as well as preventing or treating associated symptoms. In the past, mediastinal surgery was associated with the need of the widest possible exposure, which was achieved through a median sternotomy or thoracotomy. In the early 1990s, minimally invasive techniques began to demonstrate at least the same effectiveness and clear advantages over open procedures [8].
Video-assisted thoracic surgery (VATS) has been used to treat mediastinal teratomas with good results, which mainly depend on the tumor size and existence of adhesions [9]. Tian and colleagues reported that only 11.7% of patients with tumors >10 cm were treated by VATS in their case series. VATS is associated with lower blood transfusion requirements, less postoperative pain, shorter hospital stay, better cosmetic results and lower total costs per hospitalization [10, 11]. Its use and safety have been discussed for resection of large teratomas (>10 cm) [11] regarding the conversion rate to thoracotomy due to the presence of adhesions and difficulty dissecting the blood vessels involved. Recent studies [10, 12] have shown the efficacy of VATS for resection of large tumors, demonstrating it is a safe procedure that improves postoperative prognosis of the patient. The postoperative prognosis is usually good. Studies with long-term follow-up have reported no recurrence of the disease [2, 8].



