-
PDF
- Split View
-
Views
-
Cite
Cite
Anzel Jansen van Rensburg, Andrew Riddell, A case report of ductal carcinoma of the breast metastasizing to the bowel, Journal of Surgical Case Reports, Volume 2021, Issue 10, October 2021, rjab471, https://doi.org/10.1093/jscr/rjab471
Close - Share Icon Share
Abstract
Breast cancer is one of the most common cancers affecting women. Frequent metastatic sites include liver, lungs and bone. Gastrointestinal metastases are a rare entity. We report a case of ductal carcinoma metastasizing to the sigmoid colon.
A 74-year female was found to have a mass at her sigmoid colon on surveillance colonoscopy. The initial histology showed poorly differentiated carcinoma. Further immunohistochemical staining revealed poorly differentiated metastatic ductal breast carcinoma 27 years after her primary breast cancer. She proceeded to resection and had an uneventful recovery. She remains alive with stable retroperitoneal lymph node and tail of pancreas metastatic disease.
INTRODUCTION
Breast cancer accounts for the most common neoplasm to affect women and the second most common cancer in Australia. In 2020, there were 19,498 females diagnosed with breast cancer and 150 males [1]. Breast cancer is the fifth leading cause of cancer deaths within Australia and the second most common cause of death from cancer among females. Frequent metastatic sites include liver, lungs and bone. Metastasis to the gastrointestinal tract is a rare entity. We describe a case of a 74-year female that presents with metastatic breast cancer 27 years after initial diagnosis.
CASE PRESENTATION
A 72-year female was initially diagnosed with early left-sided breast cancer in 1991. She proceeded to a wide local excision and axillary lymph node clearance with histology showing a moderately differentiated ductal carcinoma. Postoperatively she proceeded to radiation treatment only. In 1996, she was diagnosed with bony metastasis. Her treatment was changed to Tamoxifen until 2001 and then ceased. Surveillance imaging in 2004 showed progression of possible ovarian lesions and the patient proceeded to hysterectomy and bilateral salpingo-oophorectomy. Histology confirmed metastatic poorly differentiated ductal carcinoma of the breast, estrogen (ER) and progesterone (PR) positive. Her treatment was then changed to aromasin and ceased in 2013. She continued clinical follow-up. Surveillance imaging then detected a left-sided retroperitoneal mass in July 2016, which was presumed to be metastatic disease and the patient was restarted on aromasin.
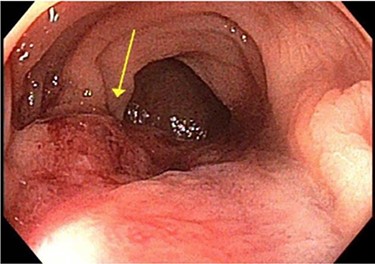
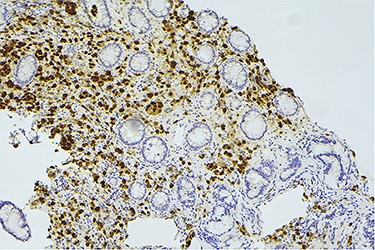
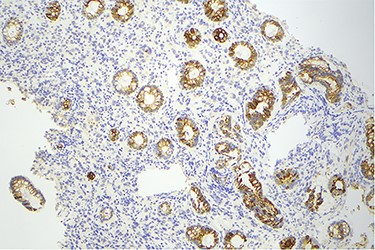
Surveillance colonoscopy in 2018 identified a fungating nonobstructing mass in the sigmoid colon (Fig. 1). Histology from a biopsy showed poorly differentiated carcinoma (Fig. 2). Given the history of breast cancer, further immunohistochemical staining was performed, which was positive for E-cadherin (Fig. 3), ER (Fig. 4), PR, GATA3 binding protein (GATA 3) (Fig. 5) and negative for Cytokeratin 20 (CK20) (Fig. 6). This confirmed metastatic invasive ductal carcinoma of breast. A positron emission tomography (PET) scan showed only the retroperitoneal mass involving the proximal sigmoid colon with no other evidence of metastatic disease (Fig. 7).
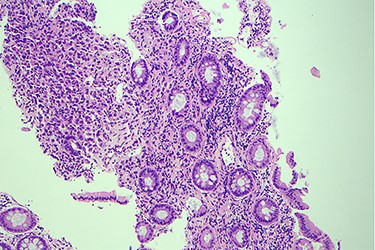
Histology slide of the biopsy with H&E staining showing poorly differentiated carcinoma.
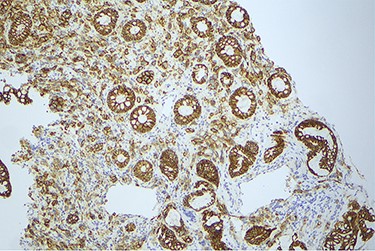
Histology slide showing positive immunohistochemical staining for E-cadherin.
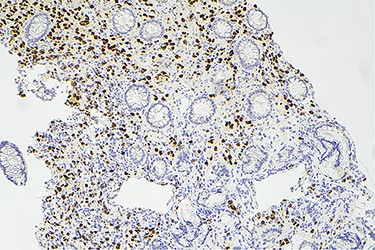
Histology slide showing positive immunohistochemical staining of estrogen receptor.
Histology slide showing positive immunohistochemical staining for GATA receptor.
Histology slide showing CK20 staining of colon epithelium, however, there is no uptake in the tumor cells.
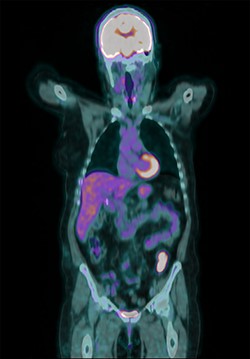
PET scan showed only the retroperitoneal mass involving the proximal sigmoid colon with no other evidence of metastatic disease.
The patient proceeded to a laparoscopic anterior resection with histology showing metastatic invasive ductal carcinoma of breast with lymphovascular and perineural invasion. Fourteen of the seventeen lymph nodes showed metastatic disease with extra nodal extension, ER/PR positive and HER-2 negative.
By the patient’s choice, she remained on aromasin therapy. Repeat colonoscopy in July 2018 showed no recurrence.
Staging CT chest abdomen and pelvis in July 2019 showed a new nodule adjacent to the tail of pancreas, new para-aortic lymphadenopathy, and suspicious lesions in segment 7 of the liver. There was no evidence of bony metastasis. Her CA15.3 increased from 37 to 51. The patient was offered chemotherapy; however, she declined. Her treatment was then changed to Letrozole therapy. There was local progression of para-aortic lymphadenopathy causing obstruction of left ureter requiring a stent in June 2021. Her treatment was changed to include Palbociclib as well as Letrozole.
Currently, the patient’s metastatic disease remains stable. She has done remarkably well to survive this far and continues to remain relatively asymptomatic.
DISCUSSION
Breast cancer is the most common neoplasm to affect women, affecting up to 32% with ductal carcinoma being the most common type of invasive breast cancer [1]. The most common sites for metastatic breast cancer include regional lymph nodes, liver, bone and brain [2]. The gastrointestinal system is a rare site for metastatic disease. Lobular carcinoma is more commonly seen to metastasize to gastrointestinal tract (GIT) despite the higher prevalence of ductal carcinoma. This was evident in the literature with several studies, including a case series by Taal et al. and Borst and Ingold, showing a predominance of lobular carcinoma metastasizing to the colon and rectum [3–4]. There are only a small number of reported cases of ductal carcinoma metastasizing to the colon and even fewer to the rectum [4]. Borst and Ingold found of 2605 breast cancer cases with metastatic disease, lobular carcinoma accounted for 359 cases, whilst ductal carcinoma accounted for 2246. Of these cases, only 4.7% were to the GIT with ductal carcinoma only accounting for 0.2%.
A retrospective study by McLemore et al found 23 cases of breast cancer with gastrointestinal metastasis, of these 8% spread to the esophagus, 28% to the stomach, 19% to the small bowel and 45% to the colon and rectum [5]. Metastatic disease to gastrointestinal and gynecological systems, peritoneum and retroperitoneum is more commonly seen in lobular carcinoma compared to ductal carcinoma, which is more commonly seen to involve liver, lung and brain.25
The literature reveals varying intervals between diagnosis of primary breast cancer and the detection of metastatic gastrointestinal disease. A mean interval of seven years between primary cancer and manifestations of metastatic disease was reported by Mclemore et al. [5] Whilst other cases report metastasis more than 20 years later including this case [7–8].
Histological examination often involves multiple markers to further assist in the diagnosis. According to the literature, helpful markers include GCDFP-15, ER, PR and GATA-3 [5, 9]. Expression of CK-7 and absence of CK-20 is also commonly seen in ductal carcinoma [10]. The immunohistochemical profile for our case was positive for E-cadherin, CK-7, ER, GATA-3 and negative for CK-20 and CDX2.
Metastatic disease to the colon in breast cancer patients can present with no symptoms or non-specific symptoms. From the literature, possible symptoms can include abdominal pain, vomiting, melaena, weight loss, fatigue and a palpable mass [5]. It is therefore important that it is considered as a differential as early detection is vital to allow intervention.
The treatment for these patients will depend on the presentation. In the situation of an acute surgical abdomen secondary to metastatic disease, surgery usually prevails. Often the final diagnosis of metastatic breast cancer is not known until histology is returned. Chemotherapy or systemic hormonal treatment alone or as an adjunct to surgery has shown to provide favorable outcomes for those with metastatic breast cancer to bowel. Unfortunately, survival is poor for those diagnosed with the average survival being 12–16 months [3, 11].
References
- immunohistochemistry
- lung
- cancer
- colonoscopy
- infiltrating duct carcinoma
- intestines
- neoplasm metastasis
- sigmoid colon
- breast
- histology
- liver
- breast cancer
- undifferentiated carcinoma
- surveillance, medical
- retroperitoneal lymph node
- pancreas tail
- breast carcinoma
- secondary malignant neoplasm of gastrointestinal tract



