-
PDF
- Split View
-
Views
-
Cite
Cite
Ikenna Anderson Aneke, Thiruendran Gunendran, The role of vitamin K in the non-operative management of bilateral adrenal hemorrhage on a background of antiphospholipid syndrome and coagulopathy: a case report, Journal of Surgical Case Reports, Volume 2021, Issue 10, October 2021, rjab440, https://doi.org/10.1093/jscr/rjab440
Close - Share Icon Share
Abstract
Bilateral adrenal hemorrhage (BAH) is a rare condition, which can easily become a serious threat to life. It is even rarer in the setting of antiphospholipid syndrome (APLS), which in itself is associated with coagulopathy as well as the need for lifelong anticoagulation. Death from BAH is commonly due to adrenal insufficiency from infarction within the gland. Our case is that of a 53-year-old woman with APLS who presented to the emergency department with a markedly raised international normalized ratio and bilateral loin pain. She developed adrenal insufficiency and required glucocorticoids while on admission. Her anticoagulants were also adjusted and she received vitamin K. She made good progress thereafter and was discharged after 11 days. Vitamin K should be considered in patients with markedly deranged clotting profile and BAH to prevent ongoing bleeding. Early adrenal axis testing is also recommended to forestall delayed diagnosis of adrenal insufficiency.
INTRODUCTION
Bilateral adrenal hemorrhage (BAH) in the setting of antiphospholipid syndrome (APLS) is rare and potentially life-threatening. We report the case of a 53-year old woman with APLS on warfarin who presented with bilateral loin pain. She was found to have BAH and a very high international normalized ratio (INR). Her anticoagulation was adjusted, and she made good clinical progress.
CASE REPORT
A 53-year-old woman with APLS on lifelong warfarin was referred to the urology unit. Her other comorbidities included epilepsy, primary hyperparathyroidism, previous parathyroidectomy and aortic regurgitation. She had presented to our emergency department with bilateral flank pain that started three days prior. There was no preceding history of trauma. She also had nausea, vomiting, fever and rigors. She was tender in her right renal angle at presentation and had 2+ blood in her urinalysis but no nitrites or leukocytes. She also had a C-reactive protein of 277, hemoglobin of 105 g/L and a white cell count of 8.3 x 109/L. Her estimated glomerular filtration rate was 45 ml/min/1.73m2 and she was in AKI 1 at presentation. Her INR was noted to be quite high at 11.7 with an activated partial thromboplastin time of 100.4 s and a prothrombin time of 138.2 s. She reported a nosebleed few days prior but had no other history of abnormal bleeding. In the last 7 years, her INR had exceeded her target range of 2–3 only on four occasions with the highest value being 8.4.
She had a non-contrast computed tomography (CT) of the abdomen to rule out urolithiasis. This showed features of right-sided pyelonephritis and small bilateral renal calculi but no ureteric calculi or hydronephrosis. BAH was confirmed on her triple phase renal CT scan (Fig. 1). She was started on intravenous fluids and broad-spectrum antibiotics (IV temocillin and gentamicin) to cover for suspected pyelonephritis. Her warfarin was held initially, and she was given vitamin K. Following advice from the hematologists, she was subsequently started on treatment dose of enoxaparin, but her platelet count started to decline, and this was changed to fondaparinux. On her second day on admission, she developed adrenal insufficiency evidenced by persistent hypotension, hyponatraemia of 122 mmol/L (reference range 133–146 mmol/L) and hypocortisolaemia of 40 nmol/L (reference range 100–500 nmol/L). She received intravenous hydrocortisone which was converted to oral steroids after 24 h. Her sodium level normalized by Day 8 of admission. Following 3 days of intravenous antibiotics, she was changed to oral amoxicillin, which was continued for 7 more days.
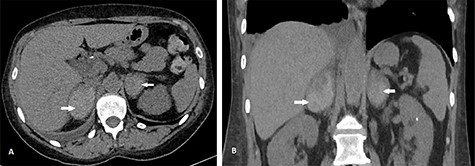
CT scan showing axial (A) and coronal (B) views of BAH (arrows). The right adrenal hemorrhage measured 35 × 52 mm axially and the left adrenal hemorrhage measured 40 × 33 mm.
She had sequential CT and ultrasound scans to monitor her adrenal hemorrhages. Adrenal artery embolization was considered in the event of a rebleed and the patient was pre-emptively counseled accordingly. Her hematomas however remained stable on her scans. She had serial hemoglobin monitoring and did not require blood transfusion. She had a heparin-induced thrombocytopenia (HIT) screen on Day 8 on admission and this was negative. She was therefore, managed conservatively and discharged after 11 days. At discharge, she was placed on a reducing dose of oral hydrocortisone to reach target maintenance doses of 10 mg in the morning, 5 mg at noontime and 5 mg at bedtime. She was discharged on fondaparinux and her warfarin was restarted after 5 days when her platelet counts normalized. She had a repeat CT scan 6 weeks post discharge, which showed slow resolution of her hematomas with no underlying mass (Fig. 2).
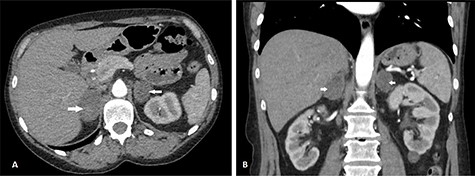
CT scan after 6 weeks showing axial (A) and coronal (B) views of resolving BAH (arrows). The right adrenal hemorrhage now measures 30 × 46 mm axially and the left adrenal hemorrhage measures 33 × 28 mm.
DISCUSSION
Spontaneous adrenal hemorrhage has an incidence of about 0.14–1.1% based on post-mortem studies [1]. Many causes of BAH have been identified, most of which stimulate the physiologic response to trauma. These include burns, severe sepsis, major trauma and major surgery. It has also been seen in bacterial infections like Haemophilus influenzae and meningococcal infection as seen in Waterhouse–Friderichsen syndrome [2]. Viruses like parvovirus B19, Epstein–Barr virus and cytomegalovirus have also been implicated. APLS is an autoimmune disorder characterized by medium-to-large vessel thrombosis occurring in the presence of antiphospholipid antibodies (aPLs). The life-threatening primary adrenal insufficiency associated with BAH has been noted in about 0.4% of patients with APLS making it quite a rare complication [3].
The vascular anatomy of the adrenal gland is unique as it is supplied by three arteries, which enter the gland and break into multiple branches forming a vascular plexus in the area of the zona reticularis. The gland is however drained by a single vein, resulting in an anatomical ‘bottle neck’ creating the perfect conditions for hemorrhage within the gland in the event of reduced outflow. Adrenal vein thrombosis is the most common pathophysiologic mechanism of spontaneous adrenal hemorrhage. It leads to gland edema resulting in arterial occlusion, ischemia as well as hemorrhagic infarction [4]. The second, rarer mechanism, is that of spontaneous adrenal bleeding that is unrelated to vascular thrombosis. This mechanism is more common in patients who are undergoing surgery or on anticoagulants [5].
Patients with BAH and adrenal infarction will most commonly present with abdominal symptoms (55% of cases). Fever, nausea, vomiting, fatigue and altered sensorium are other symptoms that patients may present with [6]. The treatment of choice for BAH on a background of APLS as suggested by most authors, is careful anticoagulation therapy with a combination of warfarin and heparin, aiming for a target INR of 2–3 [7]. In our patient however, due to her markedly raised INR of 11.7, the clinical decision to initially discontinue her anticoagulation and start vitamin K was made.
CONCLUSION
BAH should be suspected in patients with APLS presenting with abdominal pain. Adrenal insufficiency should however, be anticipated in these patient and steroids initiated early. Vitamin K therapy should also be considered. Overall, a high index of suspicion is necessary in managing this group of patients.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- anticoagulants
- anticoagulation
- antiphospholipid syndrome
- vitamin k
- adrenal glands
- hemorrhage
- blood coagulation disorders
- adrenal gland hypofunction
- glucocorticoids
- blood coagulation
- emergency service, hospital
- flank pain
- infarction
- international normalized ratio
- coagulation process
- adrenal hemorrhage
- delayed diagnosis



