-
PDF
- Split View
-
Views
-
Cite
Cite
Frank Kiwango, Alex Mremi, Albert Masenga, Huda Akrabi, Intestinal ischemia in a COVID-19 patient: case report from Northern Tanzania, Journal of Surgical Case Reports, Volume 2021, Issue 1, January 2021, rjaa537, https://doi.org/10.1093/jscr/rjaa537
Close - Share Icon Share
Abstract
Novel coronavirus disease 2019 (COVID-19) was first identified in Wuhan, China, and declared by World Health Organization as a pandemic in March 2020. Since then, it has been well known for COVID-19 patients to present with clinical manifestations of severe acute respiratory syndrome (SARS-CoV-2) similar to the influenza. However, in the course of the disease, various pathological complications of high clinical significance have remained unknown. Impaired blood supply to the visceral vascular system can cause serious life-threatening acute damage. We report a case of a 60-year-old female with difficulty in breathing and extensive acute intestinal ischemia confirmed to be associated with SARS-CoV-2 infection. The patient developed a sudden abdominal pain and succumbed shortly after admission before imaging studies were performed. Autopsy revealed massive bowel ischemia. This case highlights the importance of paying attention to serious and less known clinical manifestations other than pulmonary symptoms and fever.
INTRODUCTION
Novel coronavirus disease 2019 (COVID-19) has been identified in Wuhan, China, in December 2019 and declared by World Health Organization (WHO) as a pandemic in March 2020 [1]. Multiple cases have been identified in different parts of the world as an acute respiratory infectious disease. Clinical manifestation of COVID 19 mainly include fever, fatigue, respiratory symptoms and to a lesser extent gastrointestinal symptoms such as vomiting and diarrhea [2]. Severe cases may progress to acute respiratory distress syndrome, septic shock and multiorgan failure. As it is a relatively new disease, clinical manifestations and pathology remains incompletely understood [3].
CASE REPORT
A 60-year-old female patient, who was known to have hypertensive heart disease and diabetes mellitus, presented to our facility with a 9-day history of progressive difficulty in breathing associated with dry cough, chest pain and body malaise. She denied any recent history of fever or abdominal pain.
Upon arrival at the emergency department, she was hemodynamically unstable, saturating 85% in room air with high random blood glucose of 27.8 mmol/L. Physical examination was unremarkable.
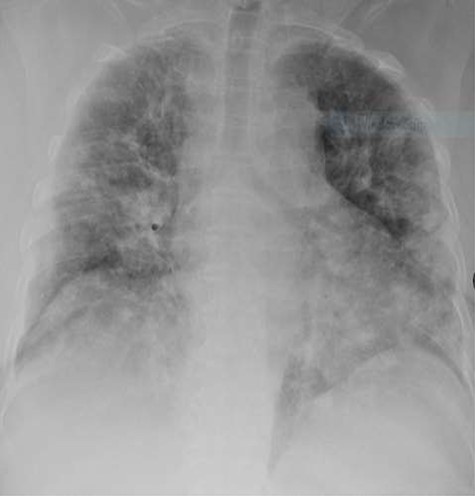
Laboratory investigations were within normal ranges except for D-dimer, which was high (Table 1). Chest X-ray showed bilateral homogeneous opacification (Fig. 1).
| WBC (3.5–9.0 × 109/L) . | Hb (10–14 g/dl) . | Platelet (150–450 × 109/L) . | Creatinine (60–120 μmol/L) . | Urea (2.1–7.1 mmol/L) . | Sodium (136–148 mmol/L) . | Potassium (3.8–5 mmol/L) . | D-dimer (0.0–0.5 μgEFU/ml) . | ASAT (<35 U/L) . | ALAT (< 35) . |
|---|---|---|---|---|---|---|---|---|---|
| 7.7 × 109/L | 12.6 g/dl | 232 × 109/L | 88 | 14.5 | 129.6 | 5.2 | 23.8 | 41.1 | 19.2 |
| WBC (3.5–9.0 × 109/L) . | Hb (10–14 g/dl) . | Platelet (150–450 × 109/L) . | Creatinine (60–120 μmol/L) . | Urea (2.1–7.1 mmol/L) . | Sodium (136–148 mmol/L) . | Potassium (3.8–5 mmol/L) . | D-dimer (0.0–0.5 μgEFU/ml) . | ASAT (<35 U/L) . | ALAT (< 35) . |
|---|---|---|---|---|---|---|---|---|---|
| 7.7 × 109/L | 12.6 g/dl | 232 × 109/L | 88 | 14.5 | 129.6 | 5.2 | 23.8 | 41.1 | 19.2 |
WBC, white blood cell; Hb, hemoglobin; FEU, fibrinogen equivalent unit; ASAT, aspartate aminotransferase; ALAT, alanine aminotransferase.
| WBC (3.5–9.0 × 109/L) . | Hb (10–14 g/dl) . | Platelet (150–450 × 109/L) . | Creatinine (60–120 μmol/L) . | Urea (2.1–7.1 mmol/L) . | Sodium (136–148 mmol/L) . | Potassium (3.8–5 mmol/L) . | D-dimer (0.0–0.5 μgEFU/ml) . | ASAT (<35 U/L) . | ALAT (< 35) . |
|---|---|---|---|---|---|---|---|---|---|
| 7.7 × 109/L | 12.6 g/dl | 232 × 109/L | 88 | 14.5 | 129.6 | 5.2 | 23.8 | 41.1 | 19.2 |
| WBC (3.5–9.0 × 109/L) . | Hb (10–14 g/dl) . | Platelet (150–450 × 109/L) . | Creatinine (60–120 μmol/L) . | Urea (2.1–7.1 mmol/L) . | Sodium (136–148 mmol/L) . | Potassium (3.8–5 mmol/L) . | D-dimer (0.0–0.5 μgEFU/ml) . | ASAT (<35 U/L) . | ALAT (< 35) . |
|---|---|---|---|---|---|---|---|---|---|
| 7.7 × 109/L | 12.6 g/dl | 232 × 109/L | 88 | 14.5 | 129.6 | 5.2 | 23.8 | 41.1 | 19.2 |
WBC, white blood cell; Hb, hemoglobin; FEU, fibrinogen equivalent unit; ASAT, aspartate aminotransferase; ALAT, alanine aminotransferase.
The patient was then admitted to the isolation ward and COVID-19 polymerase chain reaction tested positive; hence, the final diagnosis was COVID-19 infection. Three days after admission, she started complaining of sudden onset of abdominal pain with no other gastrointestinal symptoms. On abdominal examination, tenderness in the epigastric area was the only positive finding. It was temporarily relieved by pantoprazole. The following day, the patient complained of severe cramping abdominal pain. Urgent abdominal ultrasound (USS) was ordered; however, before the USS was performed, the patient started to desaturate on oxygen therapy. Advanced Cardiovascular Life Support protocol was initiated and 30 min later the patient had no signs of life.
As the cause of death was not identified, autopsy was requested and revealed massive large bowel ischemia without perforation (Fig. 2) and with multiple foci of pulmonary infarcts.

Histopathology analysis of the lung specimens revealed mixed chronic inflammatory infiltrates associated with pulmonary vascular thrombosis and areas of extensive necrosis (Figs 3 and 4). Bowel tissue sections revealed severe ischemic necrosis and mesenteric vessel thrombosis (Fig. 5). Thus, the primary causes of death were ruled to be ischemic colitis and pulmonary thrombosis due to COVID-19. The underlying disease conditions contributing to the cause of death being hypertensive heart disease, diabetes mellitus and septicemia.
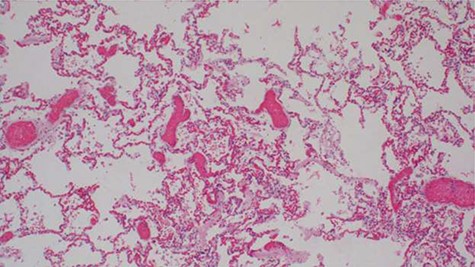
Histopathology of lung tissue showing mixed chronic inflammatory infiltrates and vascular thrombosis (hematoxylin and eosin ×100).
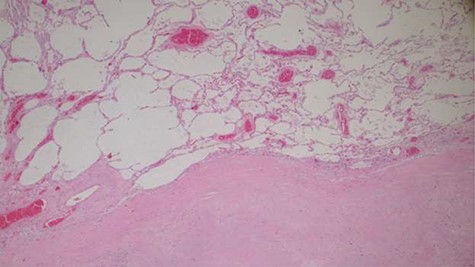
Histopathology of lung tissue showing vascular thrombosis and extensive fibrosis and necrosis (hematoxylin and eosin ×40).
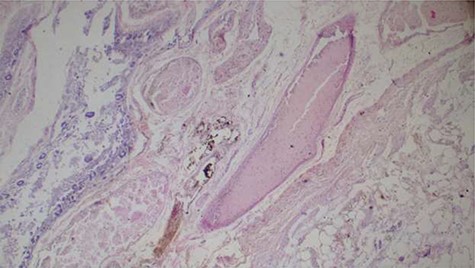
Histopathology of the bowel tissue showing ischemic necrosis and the vascular thrombosis (hematoxylin and eosin ×100).
DISCUSSION
Our report of acute intestinal ischemia in a confirmed patient of COVID-19, despite having low risk factors for ischemic bowel disease, indicates various aspects of the disease that are still not well documented and should be considered. In addition to affecting the respiratory tract, the disease can cause thrombogenic ischemia in various parts of the body, including the gastrointestinal tract. Currently, our clinical understanding of the entire manifestations and complications of COVID-19 is still evolving.
WHO declared COVID 19 as a pandemic in late March 2020 [1]. Since then, COVID has been a public health emergency and had a massive public health effect globally [2]. The disease has a wide range of clinical manifestations, ranging from asymptomatic to life-threatening symptoms [2]; therefore, making the diagnosis and management are challenging, particularly to the patients who are asymptomatic [3].
Among the major symptoms reported from various studies are pulmonary symptoms [4]. However, the patients may also present with gastrointestinal symptoms such as nausea, abdominal pain, diarrhea, vomiting [3–5] and isolated gastrointestinal symptoms [4]. There is evidence that COVID-19 invades the gastrointestinal tract, which can lead to intestinal ischemia and this condition can be due to hypercoagulable state. Patients report to have severe abdominal pain with hyperactive bowel sounds followed by paralytic ileus, which can limit blood circulation; hence, thrombosis in the intestine leading to intestinal ischemia [1, 6–9].
Increase in D-dimer levels and being diabetic have shown to predispose the patients to high risk of thrombosis [1, 10]. Our patient had both risk factors of having high D-dimer levels and being diabetic [1, 10]. Reports have described coagulopathy as a common complication in patients with severe COVID-19 [6–9]. Several observational studies have reported elevated baseline D-dimer levels in patients hospitalized for moderate to severe COVID-19. These elevated baseline D-dimer levels have been associated with disease severity and mortality in retrospective cohorts [6].
Ischemic colitis is a condition resulting from decreased blood supply to the colon, leading to mucosal injury, cellular ischemia and necrosis. Treatment for ischemic colitis mainly involves supportive care with bowel rest and close observation if there is no evidence of perforation, necrosis or gangrene. Surgical intervention with colonic resection is indicated if imaging shows colon infarction and necrosis or for patients with right-sided colon involvement [9, 10]. Anticoagulation is rarely indicated. Our patient’s condition changed suddenly before the imaging investigations and unfortunately succumbed shortly afterwards.
COVID-19 is a relatively new disease with emerging new evidences. Despite pulmonary symptoms being the lead, gastrointestinal symptoms are emerging and can indicate a serious complication such as intestinal ischemia. Hence, early imaging should be considered in order to further strengthen the early detection and early intervention to reduce the mortality rate as much as possible. Autopsy examination is an invaluable tool in attempts to understand the pathobiology of the disease.
ACKNOWLEDGMENTS
The authors thank the patient’s son for providing the consent for this publication. The authors also thank Dr Sarah Urassa, the director of hospital services, for her support.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
ETHICAL APPROVAL
No approval required.
CONSENT
Written and signed consent was obtained from the patient’s son to perform autopsy and to use for further academic platforms.
GUARANTOR
All the authors are the guarantors of this paper as F.K., A.M. and H.A. managed the patient, collected all clinical information and wrote the manuscript. A.M. performed the autopsy and histological analyses. All authors read, edited and approved the final manuscript.
References
- gastrointestinal tract vascular insufficiency
- influenza
- respiration
- abdominal pain
- vascular insufficiency of intestine, acute
- vascular flow
- inspiration
- fever
- autopsy
- china
- signs and symptoms
- signs and symptoms, respiratory
- tanzania
- world health organization
- infections
- diagnostic imaging
- vascular system
- severe acute respiratory syndrome
- vasculature
- pandemics
- blood supply, arterial
- sars-cov-2
- covid-19



