-
PDF
- Split View
-
Views
-
Cite
Cite
Alberto Testori, Marco Alloisio, Umberto Cariboni, Francesco Costa, Emanuele Voulaz, Edoardo Bottoni, Matilde De Simone, Daoud Rahal, Ugo Cioffi, Voluminous schwannoma type ‘ancient’ of the cervicothoracic district removed through a cervicotomic approach, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa402, https://doi.org/10.1093/jscr/rjaa402
Close - Share Icon Share
Abstract
Schwannomas are generally benign tumors, well delimited, resulting from nerve sheaths that are frequently found in the thorax, mainly in the posterior mediastinum. We report a 58-year-old patient who carried out investigations following the appearance of a large right supraclavicular cervical mass associated with anisocoria and eyelid ptosis, histologically diagnosed as ancient schwannoma, completely removed through a cervicotomic approach without opening the chest.
INTRODUCTION
Schwannoma is a slow-growing benign tumor that originates from lining cells of the nerve sheath. Smaller tumors are solid, whereas larger ones may present necrosis and hemorrhagic degeneration [1]. They are called ancient schwannomas when they show an unusual growth with regressive changes [2]. We report a female patient with a large supraclavicular cervical mass that caused some neurological disorders including anisocoria and ptosis of the right eyelid, histologically diagnosed as cervicomediastinal ancient schwannoma, removed exclusively from cervicotomic approach without opening the chest.
CASE REPORT
A 58-year-old female smoker with a history of cosmetic surgery complained of a large supraclavicular cervical mass associated with some neurological disorders (including anisocoria and ptosis of the right eyelid) since 2014. An ultrasound of the neck with cytological examination raised the suspicion of ‘Schwannoma’ with liquid content. Computed tomography (CT) of the neck and chest confirmed the presence of a 6.6 × 6 cm paracervical and paramediastinal right mass that dislocated the trachea and esophagus. The injury was also confirmed by nuclear magnetic resonance imaging (MRI) of the neck and chest (Figs 1, 2).
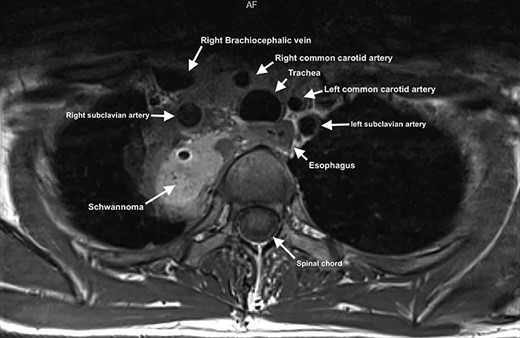
MRI showing paravertebral neurinoma with liquid content (C7-D3) with right intrathoracic involvement compressing the mediastinal structures without signs of vascular infiltration.
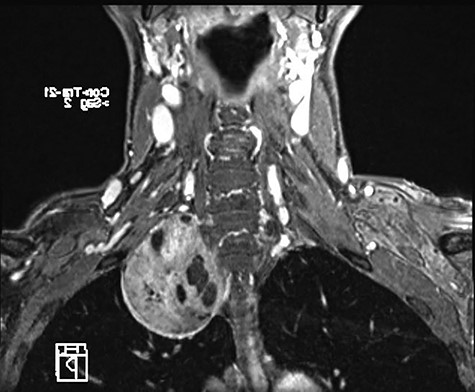
MRI of paracervical neurinoma in the coronal projection affecting the right paravertebral structures.
The patient underwent a complete removal of the mass through an exclusively cervicotomic approach (Fig. 3). The operation was performed by the thoracic surgeon and neurosurgeon who, with the help of the electron microscope, completed the operation by radically freeing the mass from the brachial plexus.
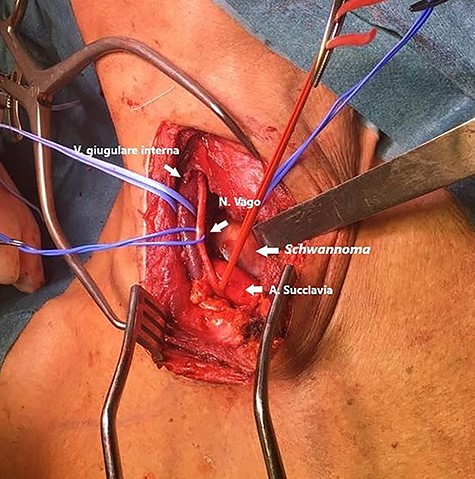
Right cervicotomic surgical approach showing the internal jugular vein, subclavian artery and vagus nerve. The lesion in its cervical portion is also visible.
Tumor was largely composed of multiple irregular yellow fragments ranging between 1 and 4 cm. The histological examination confirmed the benign characteristic of the lesion with tumor cells spindled and arranged in short bundles and vague whorls with indistinct borders and forming rows of parallel nuclei around a central zone rich in eosinophilic fibrillary processes (Verocay bodies). The cells were diffusely immunoreactive for S100 as well as SOX10 and had low proliferative index (Ki67 <1%) without necrosis or mitotic figures (Fig. 4). Focal stromal degenerative changes characterized by hyalinization areas rich in ectatic blood vessels with thickened walls were also consistent with ancient schwannoma. The patient was discharged on the second postoperative day without pain requiring non-steroidal anti-inflammatory drugs (NSAIDs). At 2 years of follow-up with clinical examination and contrast MRI (every 6 months), the patient showed a normal course with no signs of recurrence.
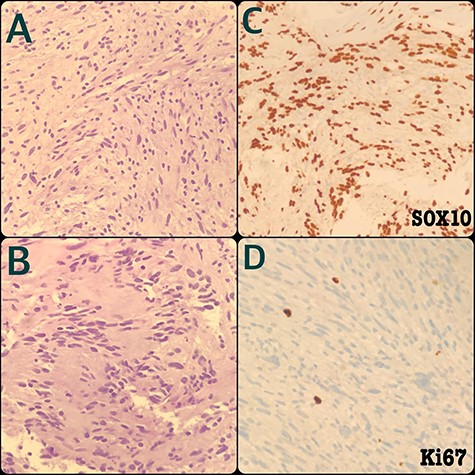
Schwannoma tumor cells are mostly spindled and arranged in short fascicles or vague whorls with indistinct cell edges (A) and sometimes for parallel nuclei rows around a central zone rich in eosinophilic fibrillary processes (Verocay bodies) (B). The cells are diffusely immunoreactive for S100 as well as SOX10 (C) and have low proliferative index (Ki67 <1%) without necrosis or mitotic figures (D).
DISCUSSION
Schwannomas are encapsulated benign tumors that originate from Schwann cells of cranial, peripheral or autonomic nerve sheaths. It was first described in 1908 by Verocay who coined the term neurinoma in 1910, followed by Stout who used the term neurilemmoma in 1935 [3]. About 25–45% of schwannomas is located in the head and neck region. These benign lesions enter the differential diagnosis with lymphangiomatous malformations, capillary lymphangioma and cystic hygroma. It is very rare to find a schwannoma of the brachial plexus; in fact, the most common benign tumor of the peripheral nerve sheath (PNST) deriving from the brachial plexus is the neurofibroma, which is usually associated with type I neurofibromatosis [3]. Schwannomas are the second most common PNST, of which only 5% derive from the brachial plexus. Schwannomas affect both sexes equally and generally occur in patients over the age of 40 as indolent solitary masses [3, 4]. Patients may experience symptoms of nerve compression and less commonly they may experience radiating pain and sensory or motor impairment. Back pain is extremely rare. Neurogenic tumors typically arise in the posterior mediastinum and rarely in the middle mediastinum. CT and MRI can be useful in confirming tumor extension and resectability [5, 6], but only histological examination can be able to define an exact diagnosis [5]. They macroscopically present themselves as roundish, oval or plexiform masses with a color that varies from yellow to gray. Contrary to neurofibromas, schwannomas can show areas of cystic degeneration and hemorrhagic necrosis. Histologically, schwannomas are lesions composed of following two components: a highly cellular component (Antoni A) and a mixoid component (Antoni B). Tumors with exclusively areas of Antoni A are also called cell neurilemmomas and can be confused with malignant fibrosarcomas or schwannomas. In schwannomas with prevalent Antoni B areas, the differential diagnosis must be made with macrocystic mucinous tumors and lymphangiomas [1]. Malignant schwannomas generally have a wide perineural and intraneural spread. The goal of treatment is complete tumor resection with nerve conservation. As schwannomas are well encapsulated, it is almost always possible to enucleate and separate the tumor from the nerve sheath. To our knowledge, only six cases of ancient schwannomas have been published in female patients, ours is the seventh case reported in English literature [7]. Ours is the first case of cervicomediastinal schwannoma completely removed through a cervicotomic approach without opening the chest, and with the collaboration of a neurosurgeon equipped with an electron microscope. The cervicotomic removal allowed a discharge in second postoperative day without any pain requiring NSAIDs, and with better esthetic wound results. Courvoisier [8] reported the first surgical excision of a schwannoma of the brachial plexus in 1886, complicated by the paralysis of the deltoid and biceps muscles. The complications reported in most cases are temporary sensory and motor deficits.
CONCLUSION
After a careful study of the patient with CT–MRI and cytohistological examination, surgical excision should be the best treatment choice for schwannomas that cause neurological deficit, discomfort or are characterized by continuous growth with the suspicion of malignancy.
ACKNOWLEDGMENT
The authors thank Dr Gerardo Cioffi, native speaker, for reviewing the English language.
CONFLICT OF INTEREST
None declared.
FUNDING
None.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available on request.
AUTHORS’ CONTRIBUTION
All authors carried out the concept and the design of the study and revised the manuscript.



