-
PDF
- Split View
-
Views
-
Cite
Cite
Adam R Dyas, David Thor Johnson, Erin Rubin, Richard D Schulick, Piyush Kumar Sharma, Yttrium-90 selective internal radiotherapy as bridge to curative hepatectomy for recurrent malignant solid pseudopapillary neoplasm of pancreas: case report and review of literature, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa325, https://doi.org/10.1093/jscr/rjaa325
Close - Share Icon Share
Abstract
Recurrent malignant solid pseudopapillary neoplasms of the pancreas (SPNP) are rare tumors with unpredictable clinical and histopathological features. There is a lack of consensus regarding utilization of adjuvant modalities in conjunction with or in lieu of curative metastatectomy. We present a remarkable case where Yttrium-90 selective internal radiation therapy (Y-90 SIRT) was successfully utilized to elucidate underlying tumor biology and aid resection of a large multifocal recurrent metastatic SPNP in the right hemi-liver of a 59-year-old female. Thus, in cases where curative metastatectomy remains the treatment goal in management of recurrent and/or metastatic SPNPs, Y-90 SIRT is a safe and effective adjunct treatment to facilitate curative resection.
INTRODUCTION
Solid pseudopapillary neoplasms of the pancreas (SPNP) represent a rare form of exocrine pancreatic tumor with well-documented predisposition in young women. These typically present with abdominal pain and have a pathognomonic appearance on imaging as large encapsulated masses with intra-tumoral hemorrhage. Prognosis is excellent with reported survival at 5 years being >95% with optimal surgical resection but aggressive behavior has been reported in some cases especially with male sex, vascular invasion, extra-pancreatic invasion, nodal metastasis, and Ki67 index > 4% [1]. In the latter group the disease-specific survival is significantly poorer with 5-year survival reported to be around 35% [2] and more importantly, absence of these features, does not preclude aggressive behavior. Nevertheless, aggressive surgical metastatectomy remains the standard of care with excellent long-term survival.
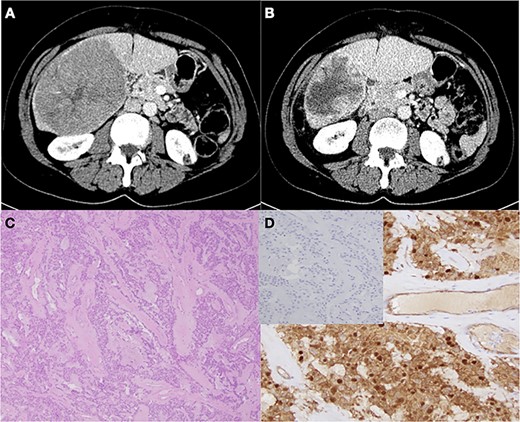
CT imaging of metastatic recurrent SPNP in right hepatic lobe before (A) and after (B) Y-90 treatment. (C) Characteristic pseudopapillae with hyaline stroma (H&E staining, ×4 magnification). (D) Confirmatory β-catenin immunostaining with negative chromogranin A staining (inset)
We present an interesting case of SPNP with metachronous hepatic metastasis despite an R0 index resection, lack of histological features suggestive of aggressive behavior and long recurrence free interval. The presence of bulky liver metastasis with satellitosis and associated portocaval lymphadenopathy added an extra layer of complexity to the surgical management and merit discussion as there are no evidence-based guidelines to direct decision making in this context.
CASE REPORT
A 59-year-old female presented with a 7.6 × 9.7 cm heterogeneous mass involving the tail and body of the pancreas in 2008. Since, the patient was undergoing evaluation for a lymphoma in light of a recently discovered forehead lesion, an endoscopic ultrasound guided biopsy was performed to rule out an alternative diagnosis which confirmed the mass to be SPNP. She underwent a distal pancreatectomy and splenectomy with segmental transverse colectomy and negative surgical margins. She recovered well from her operation and did not show any evidence of recurrence up until December 2011, after which she was lost to follow up.
She presented again in November 2018 with a 3-month history of progressive right upper quadrant abdominal pain. Computed tomography (CT) imaging revealed a large hypoattenuating 10.3 × 12.7 × 9.8 cm3 lesion in the right hemi-liver, with multiple satellite lesions (Fig. 1A). There was no radiographic evidence of vascular invasion but extensive portocaval lymphadenopathy was noted. Liver core needle biopsy was consistent with recurrent solid pseudopapillary neoplasm. After a multidisciplinary discussion, it was recommended that she undergo Yttrium-90 selective internal radiation therapy (Y-90 SIRT) prior to resection and she received 118.4 Gy of treatment dose from a single administration of Theraspheres in January 2019. Posttreatment surveillance imaging in April revealed a remarkable interval decrease in size of the dominant mass to 8.3 × 6.4 × 7.1 cm3 without identification of any new lesions and stable lymphadenopathy (Fig. 1B). Given the favorable response to SIRT, long progression free interval and her excellent clinical status, an open extended right hepatectomy and portocaval as well as left renal vein lymphadenectomy were performed. Notably, extensive sclerosis and fibrotic reaction secondary to the Y-90 treatment made the portal dissection more challenging, but very accomplishable. She tolerated the procedure well and after a week in hospital was discharged home. Final pathology was consistent with multifocal solid pseudopapillary tumor, with negative margins and no evidence of tumor cells in the lymph nodes examined (Fig. 1C,D). There was visible treatment response with 50% residual tumor viability. She remains symptom free without any evidence of residual or recurrent disease.
DISCUSSION
Local recurrence or metachronous metastasis after radical resection of SPNP have been reported in 15% of the cases and liver is the most commonly involved organ. This is likely an underrepresentation because no evidence-based recommendations regarding postoperative surveillance exist. Based on systematic review of reported cases, the mean follow-up duration falls way short of the time to recurrence and two-thirds of the patients have a surveillance period < 5 years [3]. There are documented instances of metastatic progression in the liver even after a hepatic metastatectomy and therefore a multidisciplinary evaluation before undertaking a major liver resection is warranted.
There is conspicuous paucity of data regarding utilization of adjuvant treatment of metastatic SPNP when metastatectomy is either technically complex or not feasible. Unlike in patients with metastatic pancreatic adenocarcinoma, the role of systemic chemotherapy in this setting is unclear with conflicting reports and absence of high-quality data to carry out any meaningful systematic meta-analysis. Other modalities which have been employed with varying degrees of success include liver transplantation [4], intensity modulated radiation therapy (IMRT) [5], selective internal radiotherapy (SIRT) [6], radiofrequency ablation (RFA) [7] and even hyper thermic intraperitoneal chemotherapy [8].
Transarterial chemoembolization (TACE) and transarterial embolization (TAE) are commonly used for a variety of hepatic tumors and metastatic lesions but their use in SPNP metastasis has largely remained unexplored. Matsuda et al. [9] utilized TACE in combination with systemic combination chemotherapy (5-fluorouracil, doxorubicin and mitomycin-C) with palliative intent in a patient with bilobar hepatic metastasis. They performed chemoembolization using doxorubicin in the right hemi-liver and intra-arterial infusion of doxorubicin alone in the left hemi-liver. Following this, the right-sided lesions decreased in volume (mean reduction 28%, range 13–54%), while the left-sided lesions showed an increase in size. Prasad et al. [10] reported a similar case where a 40-year-old female presented with widespread bilobar hepatic metastasis 4 years after undergoing a distal pancreatectomy for SPNP. She underwent TACE with gemcitabine and lipiodol followed by gel foam embolization and had 90% reduction in size and enhancement of the lesions on repeat imaging performed a month after treatment.
We opted to perform Y-90 SIRT prior to surgical resection because the extensive involvement of the right hemi-liver mandated a formal large hepatectomy and it was deemed imperative to rule out occult metastatic lesions in the remaining liver prior to a large parenchymal resection. Furthermore, the ensuing compensatory left hemi-liver hypertrophy decreased the risk of post-hepatectomy liver insufficiency. It can be argued that any potential technical advantage derived from the reduction in tumor volume was countervailed by the post-SIRT inflammatory changes, which made the portal dissection more exacting. Nevertheless, this case illustrates that since long-term survival with metastatectomy is the rule rather than exception, use of TACE or any adjunct modalities may be employed safely and effectively as a bridge to surgical metastatectomy.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



