-
PDF
- Split View
-
Views
-
Cite
Cite
Sena Horiguchi, Takeshi Fujita, Koji Kinoshita, Katsumi Doi, Tonsillectomy as an effective treatment for arthralgia of SAPHO syndrome, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa288, https://doi.org/10.1093/jscr/rjaa288
Close - Share Icon Share
Abstract
Synovitis, acne, pustulosis, hyperostosis and osteitis (SAPHO) syndrome has been proposed to describe a clinicoradiological entity manifesting in the joints, skin and bones. We describe a patient with SAPHO syndrome for whom bilateral tonsillectomy was effective for the treatment of arthralgia, which was quantified using multiple pain scales.
Introduction
Synovitis, acne, pustulosis, hyperostosis and osteitis (SAPHO) syndrome was proposed in 1987 to describe a clinicoradiological entity manifesting in the joints, skin and bones [1]. SAPHO syndrome is characterized by (i) hyperostosis or chronic recurrent multifocal osteomyelitis or (ii) other osteoarticular symptoms associated with dermatologic conditions, such as acne or palmoplantar pustulosis (PPP).
There are several treatment options for SAPHO syndrome, but due to the rarity of the syndrome, official therapeutic algorithms do not exist. Non-steroidal anti-inflammatory drugs are commonly administered as first-line treatment for pain relief or during the diagnostic phase, but in most cases, they are insufficient. Second-line agents include bisphosphonates, steroids and disease-modifying anti-rheumatic drugs such as methotrexate, but a significant percentage of patients fail to achieve remission. Recently, tumor necrosis factor (TNF)-α has been shown to play a role in osteitis, which may support biologics targeting TNF-α as favorable for the treatment of SAPHO syndrome. However, the occurrence of osteoarticular or skin disease worsening or showing a lack of response to anti-TNF-α drugs has been reported, and among responders, many achieve only partial control of the disease [2–4].
Pustulotic arthro-osteitis (PAO) is a joint comorbidity of PPP, most often affecting the clavicles, sternum and sternoclavicular joints. PAO is regarded as the same entity as SAPHO syndrome [5]. Recently, tonsillectomy has been reported to be extremely effective for PPP and PAO [6].
We describe a patient with SAPHO syndrome for whom bilateral tonsillectomy was effective for the treatment of arthralgia, which was quantified using multiple pain scales, including the visual analog scale (VAS), revised version of the short-form McGill Pain Questionnaire (SF-MPQ-2) and pain disability assessment scale (PDAS).
MATERIALS AND METHODS (PAIN SCALES)
Visual analog scale (VAS)
The VAS is a unidimensional measure of pain intensity, which has been widely used in diverse populations [7]. For pain intensity, the scale is anchored by “no pain” (score of 0) and “pain as bad as it could be” or “worst imaginable pain” (score of 100).
Short-Form McGill Pain Questionnaire 2 (SF-MPQ-2)
The SF-MPQ-2 assesses the major symptoms of both neuropathic and nonneuropathic pain [8]. The SF-MPQ-2 includes 22 pain descriptors with four subscales: one affective and three sensory (continuous pain, intermittent pain, and predominantly neuropathic pain). All pain descriptors are rated on a 0-to-10 (none to worst possible pain) numerical rating scale according to the severity of pain perceived or experience.
Pain disability assessment scale (PDAS)
The PDAS assesses the degree to which chronic pain interferes with various daily activities [9]. It includes 20 items reflecting pain interference in a broad range of daily activities, and respondents indicate the extent to which pain interferes with each activity on a Likert scale ranging from 0 (“pain does not interfere with this activity”) to 4 (“pain interferes completely with this activity”). Scores for the total PDAS can range from 0 to 60, with higher scores indicating higher levels of pain interference.
Case Report
A-75-year old woman presented with arthralgia in both wrists, shoulders, upper limbs and ankles and complained of difficulties in walking and engaging in housework. She was diagnosed with SAPHO syndrome based on the dermatological manifestations (Fig. 1A) and thickened sternoclavicular joints (Fig. 2). Her symptoms did not respond to celecoxib, methotrexate or adalimumab, an anti-TNF-α drug. After bilateral tonsillectomy, her arthralgia and skin symptoms dramatically improved. Prior to tonsillectomy, the VAS, SF-MPQ-2 and PDAS scores were 30, 37 and 28, respectively. Three months after tonsillectomy, the methotrexate dose was reduced, and the patient showed significant improvements in her skin symptoms (Fig. 1B). The 3-month postoperative VAS, SF-MPQ-2 and PDAS scores were 20, 7 and 19, respectively. Six months after tonsillectomy, the patient no longer needed celecoxib. The VAS, SF-MPQ-2 and PDAS scores were 10, 4 and 24, respectively. Twelve months after tonsillectomy, the VAS, SF-MPQ-2 and PDAS scores were 5, 5 and 12, respectively. She could walk without the help of a stick 1 year after tonsillectomy (Fig. 3).
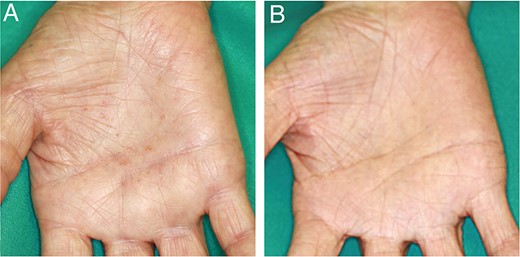
(A) Palmoplantar pustulosis appeared before tonsillectomy. (B) The pustules are disappeared 3 months after the surgery.
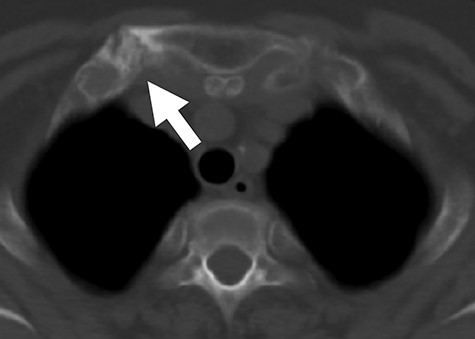
Axial CT image demonstrating thickened right sternoclavicular joint (white arrow). CT, computed tomography.
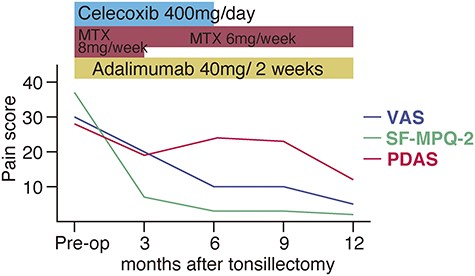
Clinical course of the patient. Three months after tonsillectomy, the methotrexate (MTX) dose could dose could be reduced from 8 to 6 mg/week. Six months after tonsillectomy, the patient no longer needed celecoxib. For pain intensity, the VAS is anchored by ‘no pain’ (score of 0) and ‘pain as bad as it could be’ or ‘worst imaginable pain’ (score of 100). The SF-MPQ-2 consists of 22 descriptors that respondents rate on a 0–10 numeric scale, with ‘0’ indicating ‘no pain’ and ‘10’ indicating ‘worst possible pain.’ Scores for the total SF-MPQ-2 can range from 0 to 220. Scores for the total PDAS can range from 0 to 60, with higher scores indicating higher levels of pain interference. VAS, visual analog scale; SF-MPQ-2, short-form McGill Pain Questionnaire-2; PDAS, pain disability assessment scale.
Discussion
We encountered a patient with SAPHO syndrome for whom bilateral tonsillectomy was effective for the treatment of arthralgia. After tonsillectomy, the patient could receive a lower dose of methotrexate and discontinue celecoxib treatment. The results of quantitative pain scales showed improvements in the patient’s pain and quality of life.
Although the pathogenesis of SAPHO remains unclear, it has been hypothesized that SAPHO syndrome represents an autoimmune and inflammatory process triggered by the breakdown of immune tolerance to resident bacteria in the tonsils [10]. It has been speculated that activated tonsillar T cells are increased by a hyperimmune response against α-streptococci (i.e. tonsil indigenous bacteria). In the tonsils of patients with PPP, such a novel immune response leads to the activation of T cells through the abnormal expression of secondary stimulation molecules, such as cytotoxic T-lymphocyte-associated protein-4, inducible co-stimulator and Smad7. These tonsillar T cells, with enhanced expression of lymphocyte antigen, CCR6 and β1-integrin–vascular cell adhesion protein-1 binding, may migrate to PPP skin lesions or affected joints and then produce sterile pustules and joint pain [6, 10]. Therefore, tonsillectomy is considered to be effective for PPP and PAO, which are related to SAPHO syndrome.
Here, we present the high efficacy of tonsillectomy in improving skin lesions and arthralgia based on multiple quantitative pain scales. Clinicians should at least present tonsillectomy as a treatment option for patients with SAPHO who do not show improvements with conventional treatment.
Conflict of interest statement
None declared.
FUNDING
None.



