-
PDF
- Split View
-
Views
-
Cite
Cite
Sílvia Rodrigues Dionísio, Eduardo Simões Ventura, Ângela Tavares Ferreira, Joana Bolinha Gonçalves, Rute Vaz Saleiro, Hugo Martins Marques, Alfredo Figueiredo Dias, Mandibular meningioma—a rare case report of a second extracranial meningioma and a systematic literature review, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa257, https://doi.org/10.1093/jscr/rjaa257
Close - Share Icon Share
Abstract
Meningiomas are benign tumours common in the central nervous system. Primary extracranial meningiomas in the jaws are extremely rare. We performed a systematic review of all the primary extracranial meningioma arising in the jawbones reported in the English-language literature including indexed and non-indexed journals and we report a unique case in our hospital of a man with two primary extracranial meningiomas, the first frontal intradiploic and 16 years later, a second located in the mandible. We found 14 cases with primary jaws meningioma and we report another one. A mandibular predominance was observed with only four cases in the maxilla. Most of them occurred in women, with a mean age of 35.9 years. It is the first published case of a patient with two primary extracranial meningiomas one of them in the mandible, which the gender, age and laterality of the lesion are less frequent.
INTRODUCTION
Meningiomas are benign tumours that are derived from the arachnoid villous structures of the meninges and are common in the central nervous system [1]. Primary extracranial meningiomas are uncommon, and in most cases occurred in glabella, bridge of the nose, skin, temporal bone, paranasal sinus and pterygopalatine fossa [1, 2]. These lesions are most often due to extension from an intracranial primary lesion and occur more infrequently in an independent fashion [3, 4]. These independent meningiomas with no association with intracranial tumours can arise in four ways. They may arise from meningocytes along the sheaths of cranial nerves when they exit the skull foramina, from fibroblastic mesenchymal cell transformation, from displaced embryonic arachnoid cells or from a metastasis from a primary central nervous system meningioma [1, 4, 5].
Primary extracranial meningiomas in the jaws are extremely rare [1, 6]. If there is no continuity with the intracranial region and no primary brain lesion present on computed tomography (CT), the mandibular lesion probably rises from transformed fibroblasts or displaced arachnoid cells [4]. Stimulation of ectopic cells or of multipotential mesenchymal cells may occur by nerve injury during a teeth extraction, or due to chronic apical inflammation that promotes the proliferation of these cells, causing tumour formation [1, 7].
The aim of this study is to identify the actual prevalence of maxillary bone meningiomas and to report a peculiar case in which the gender, age and laterality of the lesion are less frequent and the fact that it is the first published case of a patient with two primary extracranial meningiomas, one of them in the mandible.
Only 14 cases of primary extracranial meningiomas arising in the jaws have been reported in the English-language literature to date.
METHODS
We researched the MEDLINE/PubMed and Google Scholar and considered all English-language articles published since always. All articles in indexed or non-indexed journals were included in the review. The key terms used were: primary meningioma, mandibular meningioma, meningioma in the mandible and maxillary meningioma. Maxillary sinus meningiomas were excluded.
CASE REPORT
A 79-year-old man came to our department complaining of a painless swelling in the posterior region of the mandible, with uncertain beginning. The mandible in the left molar region was expanded to the buccal and lingual sides (Fig. 1). No fluctuation of the mandible or hypoesthesia of the lower lip was detected.


Panoramic radiogram and CT. A panoramic radiogram (A) and a CT (B) revealed the presence of a large and well-delineated radiolucency in the mandible.
The patient had a medical history of a frontal intradiploic meningioma, which is a subset of extradural meningioma, 16 years ago. Bifrontal craniotomy with complete tumour excision
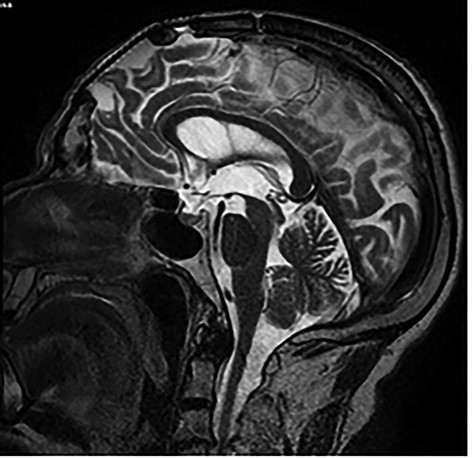
Brain MRI showing titanium cranioplasty without signs of relapse.
and cranioplasty was performed. No clinical or imaging signals of recurrence had been described. We requested a new brain magnetic resonance imaging (MRI) concluding that there was no tumour recurrence (Fig. 3).
Orthopantomography showed the presence of a large, round, well-circumscribed radiolucency in the mandible (Fig. 2A). A CT revealed an expansive lesion and a thinner cortical bone with partial interruption of the cortical margins. The mandibular canal was involved (Fig. 2B).
An incisional biopsy of the lesion revealed the presence of spindle cells and collagen bundle without atypical or mitotic figures, with a diagnosis of a transitional extracranial meningioma, similar to that of the frontal meningioma. The tumour, including the second molar, was completed removed from the mandible under general anaesthesia. After 6 months, the patient had no evidence of relapse.
RESULTS
We found 14 cases with primary jaws meningioma and we report one more (Table 1).
| First author and reference . | Age . | Gender . | Location . | Signs/symptoms . | Medical history . | Immunohistochemical markers . | Treatment . | Follow-up . |
|---|---|---|---|---|---|---|---|---|
| Landini and Kitano [5] | 48 | F | Left posterior mandibular | Painless swelling | Dental extractions 10 years before | Vimentin, EMA+ | Surgical excision | 2 years |
| Simpson and Sneddon [9] | 63 | F | Left posterior maxilla | Painless swelling | NA | Vimentin+ | Excisional biopsy | NA |
| Reddi and Strauss [11] | 26 | F | Right anterior maxilla | Swelling with facial deformity | None | Vimentin+ | Surgical excision and reconstruction with an autogenous bone graft | 2 years |
| Jones and Freedman [1] | 79 | F | Right anterior mandibular | Painless swelling | Hip replacement, angioplasty | Vimentin, EMA+ | Excisional biopsy | NA |
| Jones and Freedman [1] | 42 | F | Right posterior mandibular | Incidental finding. No symptoms. | NA | Vimentin, EMA+ | Excisional biopsy | NA |
| Kubota and Yamashiro [2] | 10 | M | Left posterior maxilla | Painless swelling | Basal cell nevus syndrome | Vimentin, EMA+ | Surgical excision | 4 years |
| Lell and Tudor [13] | 40 | F | Right posterior mandibular | Incidental finding. No symptoms | NA | Vimentin, EMA+ | Surgical excision and reconstruction with an autogenous bone graft | NA |
| Mussak and Holodny[4] | 62 | M | Left posterior mandibular | Swelling with mild pain | NA | NA | Segmental mandibulectomy and reconstruction with an autogenous bone graft | NA |
| Mosqueda-Taylor and Domínguez-Malagon [3] | 53 | F | Right posterior mandibular | Painless swelling | NA | Vimentin, EMA+ | Surgical excision | 6 months |
| Deshmukh and Rokade [14] | 18 | F | Right anterior mandibular | Painless swelling | NA | Vimentin, EMA+ | Surgical excision | 2 years |
| Pinting and Xiaofeng [12] | 59 | M | Anterior maxilla bilateral | Painless swelling | NA | Vimentin, EMA+ | Surgical excision | NA |
| Yan and Webster [6] | 35 | M | Right mandibular | Pain | None | NA | Segmental mandibulectomy | 4 months |
| Rommel and Bissinger [10] | 20 | F | Left posterior mandibular | Slight local pain | NA | Vimentin, EMA+ | Follow-up examinations without any therapeutic interventions | 1 year |
| Rege and Garcia [7] | 35 | M | Left posterior mandibular | Painless swelling | Endodontic treatment of the right second molar | Vimentin, EMA+ | Partial resection of the mandible and reconstruction with autogenous iliac tricortical bone and universal reconstruction plate | 5 years |
| Present case | 79 | M | Right posterior mandibular | Painless swelling | Primary intradiploic meningioma | NA | Surgical excision | 6 months |
| First author and reference . | Age . | Gender . | Location . | Signs/symptoms . | Medical history . | Immunohistochemical markers . | Treatment . | Follow-up . |
|---|---|---|---|---|---|---|---|---|
| Landini and Kitano [5] | 48 | F | Left posterior mandibular | Painless swelling | Dental extractions 10 years before | Vimentin, EMA+ | Surgical excision | 2 years |
| Simpson and Sneddon [9] | 63 | F | Left posterior maxilla | Painless swelling | NA | Vimentin+ | Excisional biopsy | NA |
| Reddi and Strauss [11] | 26 | F | Right anterior maxilla | Swelling with facial deformity | None | Vimentin+ | Surgical excision and reconstruction with an autogenous bone graft | 2 years |
| Jones and Freedman [1] | 79 | F | Right anterior mandibular | Painless swelling | Hip replacement, angioplasty | Vimentin, EMA+ | Excisional biopsy | NA |
| Jones and Freedman [1] | 42 | F | Right posterior mandibular | Incidental finding. No symptoms. | NA | Vimentin, EMA+ | Excisional biopsy | NA |
| Kubota and Yamashiro [2] | 10 | M | Left posterior maxilla | Painless swelling | Basal cell nevus syndrome | Vimentin, EMA+ | Surgical excision | 4 years |
| Lell and Tudor [13] | 40 | F | Right posterior mandibular | Incidental finding. No symptoms | NA | Vimentin, EMA+ | Surgical excision and reconstruction with an autogenous bone graft | NA |
| Mussak and Holodny[4] | 62 | M | Left posterior mandibular | Swelling with mild pain | NA | NA | Segmental mandibulectomy and reconstruction with an autogenous bone graft | NA |
| Mosqueda-Taylor and Domínguez-Malagon [3] | 53 | F | Right posterior mandibular | Painless swelling | NA | Vimentin, EMA+ | Surgical excision | 6 months |
| Deshmukh and Rokade [14] | 18 | F | Right anterior mandibular | Painless swelling | NA | Vimentin, EMA+ | Surgical excision | 2 years |
| Pinting and Xiaofeng [12] | 59 | M | Anterior maxilla bilateral | Painless swelling | NA | Vimentin, EMA+ | Surgical excision | NA |
| Yan and Webster [6] | 35 | M | Right mandibular | Pain | None | NA | Segmental mandibulectomy | 4 months |
| Rommel and Bissinger [10] | 20 | F | Left posterior mandibular | Slight local pain | NA | Vimentin, EMA+ | Follow-up examinations without any therapeutic interventions | 1 year |
| Rege and Garcia [7] | 35 | M | Left posterior mandibular | Painless swelling | Endodontic treatment of the right second molar | Vimentin, EMA+ | Partial resection of the mandible and reconstruction with autogenous iliac tricortical bone and universal reconstruction plate | 5 years |
| Present case | 79 | M | Right posterior mandibular | Painless swelling | Primary intradiploic meningioma | NA | Surgical excision | 6 months |
F, female; M, male; NA, not available.
| First author and reference . | Age . | Gender . | Location . | Signs/symptoms . | Medical history . | Immunohistochemical markers . | Treatment . | Follow-up . |
|---|---|---|---|---|---|---|---|---|
| Landini and Kitano [5] | 48 | F | Left posterior mandibular | Painless swelling | Dental extractions 10 years before | Vimentin, EMA+ | Surgical excision | 2 years |
| Simpson and Sneddon [9] | 63 | F | Left posterior maxilla | Painless swelling | NA | Vimentin+ | Excisional biopsy | NA |
| Reddi and Strauss [11] | 26 | F | Right anterior maxilla | Swelling with facial deformity | None | Vimentin+ | Surgical excision and reconstruction with an autogenous bone graft | 2 years |
| Jones and Freedman [1] | 79 | F | Right anterior mandibular | Painless swelling | Hip replacement, angioplasty | Vimentin, EMA+ | Excisional biopsy | NA |
| Jones and Freedman [1] | 42 | F | Right posterior mandibular | Incidental finding. No symptoms. | NA | Vimentin, EMA+ | Excisional biopsy | NA |
| Kubota and Yamashiro [2] | 10 | M | Left posterior maxilla | Painless swelling | Basal cell nevus syndrome | Vimentin, EMA+ | Surgical excision | 4 years |
| Lell and Tudor [13] | 40 | F | Right posterior mandibular | Incidental finding. No symptoms | NA | Vimentin, EMA+ | Surgical excision and reconstruction with an autogenous bone graft | NA |
| Mussak and Holodny[4] | 62 | M | Left posterior mandibular | Swelling with mild pain | NA | NA | Segmental mandibulectomy and reconstruction with an autogenous bone graft | NA |
| Mosqueda-Taylor and Domínguez-Malagon [3] | 53 | F | Right posterior mandibular | Painless swelling | NA | Vimentin, EMA+ | Surgical excision | 6 months |
| Deshmukh and Rokade [14] | 18 | F | Right anterior mandibular | Painless swelling | NA | Vimentin, EMA+ | Surgical excision | 2 years |
| Pinting and Xiaofeng [12] | 59 | M | Anterior maxilla bilateral | Painless swelling | NA | Vimentin, EMA+ | Surgical excision | NA |
| Yan and Webster [6] | 35 | M | Right mandibular | Pain | None | NA | Segmental mandibulectomy | 4 months |
| Rommel and Bissinger [10] | 20 | F | Left posterior mandibular | Slight local pain | NA | Vimentin, EMA+ | Follow-up examinations without any therapeutic interventions | 1 year |
| Rege and Garcia [7] | 35 | M | Left posterior mandibular | Painless swelling | Endodontic treatment of the right second molar | Vimentin, EMA+ | Partial resection of the mandible and reconstruction with autogenous iliac tricortical bone and universal reconstruction plate | 5 years |
| Present case | 79 | M | Right posterior mandibular | Painless swelling | Primary intradiploic meningioma | NA | Surgical excision | 6 months |
| First author and reference . | Age . | Gender . | Location . | Signs/symptoms . | Medical history . | Immunohistochemical markers . | Treatment . | Follow-up . |
|---|---|---|---|---|---|---|---|---|
| Landini and Kitano [5] | 48 | F | Left posterior mandibular | Painless swelling | Dental extractions 10 years before | Vimentin, EMA+ | Surgical excision | 2 years |
| Simpson and Sneddon [9] | 63 | F | Left posterior maxilla | Painless swelling | NA | Vimentin+ | Excisional biopsy | NA |
| Reddi and Strauss [11] | 26 | F | Right anterior maxilla | Swelling with facial deformity | None | Vimentin+ | Surgical excision and reconstruction with an autogenous bone graft | 2 years |
| Jones and Freedman [1] | 79 | F | Right anterior mandibular | Painless swelling | Hip replacement, angioplasty | Vimentin, EMA+ | Excisional biopsy | NA |
| Jones and Freedman [1] | 42 | F | Right posterior mandibular | Incidental finding. No symptoms. | NA | Vimentin, EMA+ | Excisional biopsy | NA |
| Kubota and Yamashiro [2] | 10 | M | Left posterior maxilla | Painless swelling | Basal cell nevus syndrome | Vimentin, EMA+ | Surgical excision | 4 years |
| Lell and Tudor [13] | 40 | F | Right posterior mandibular | Incidental finding. No symptoms | NA | Vimentin, EMA+ | Surgical excision and reconstruction with an autogenous bone graft | NA |
| Mussak and Holodny[4] | 62 | M | Left posterior mandibular | Swelling with mild pain | NA | NA | Segmental mandibulectomy and reconstruction with an autogenous bone graft | NA |
| Mosqueda-Taylor and Domínguez-Malagon [3] | 53 | F | Right posterior mandibular | Painless swelling | NA | Vimentin, EMA+ | Surgical excision | 6 months |
| Deshmukh and Rokade [14] | 18 | F | Right anterior mandibular | Painless swelling | NA | Vimentin, EMA+ | Surgical excision | 2 years |
| Pinting and Xiaofeng [12] | 59 | M | Anterior maxilla bilateral | Painless swelling | NA | Vimentin, EMA+ | Surgical excision | NA |
| Yan and Webster [6] | 35 | M | Right mandibular | Pain | None | NA | Segmental mandibulectomy | 4 months |
| Rommel and Bissinger [10] | 20 | F | Left posterior mandibular | Slight local pain | NA | Vimentin, EMA+ | Follow-up examinations without any therapeutic interventions | 1 year |
| Rege and Garcia [7] | 35 | M | Left posterior mandibular | Painless swelling | Endodontic treatment of the right second molar | Vimentin, EMA+ | Partial resection of the mandible and reconstruction with autogenous iliac tricortical bone and universal reconstruction plate | 5 years |
| Present case | 79 | M | Right posterior mandibular | Painless swelling | Primary intradiploic meningioma | NA | Surgical excision | 6 months |
F, female; M, male; NA, not available.
A mandibular predominance was observed with only four cases in the maxilla. Most of them occurred in women, 60%.
Ages ranged from 10 to 79 years, with a mean of 35.9 years. Eight cases developed on the right side of the jaws, six were located on the left side and one in the anterior region of the maxilla bilaterally.
In two cases the diagnosis was made incidentally and most of them had painless swelling, with the exception of two cases [8, 9].
In most cases the medical history was not relevant, except for one case, in which a 10-year-old child was diagnosed with a mandibular meningioma and 2 years after the tumour enucleation, he showed odontogenic keratocytes due to basal cell nevus syndrome. Some other cases had a history of dental treatments. In our case, medical history was important because he had an intradiplocal meningioma treated 16 years ago. We made sure that there was no relationship with the current meningioma, with no signs of recurrence shown on MRI.
In all cases on orthopantomography, a well-rounded radiolucent lesion was detected. Some did CT and MRI. However, the definitive diagnosis was with biopsy and immunohistochemical markers were useful in supporting the diagnosis [1].
Excluding Mussak and Holodny [4] and Yan and Webster [6] who only reported cytology, 100% were positive for vimentin and those who studied for the epithelial membrane antigen (EMA) marker were also positive (86%).
The treatment for jaws meningioma involved surgical excision with good results with this patient and six previous cases [1, 2, 5]. Excisional biopsy has been effective in three previous cases, and in another four cases resection preceding bone graft reconstruction was performed. The only case in which no surgical excision was performed was that of a young patient and follow-up after 12 months showed no significant progression or increase of clinical complaints [10].
DISCUSSION
Intraosseous meningiomas, which constitute <2% of meningiomas overall, are a subtype of primary extracranial meningiomas [3, 6, 12].
Most occurred in women, which is in accordance with the fact that meningiomas in general have a marked predilection for female gender. It has been postulated that hormones play a significant role in the development of these neoplasms since they commonly express progesterone receptor [3].
Meningiomas are slow growing and usually asymptomatic tumours that often shows a well-rounded radiolucent lesion in orthopantomography. This non-specific pattern urges the need to include a large number of lesions in the differential diagnosis. The slow growth observed in all cases reduces the likelihood of being a malignant or an inflammatory condition. CT and MRI features are non-specific. MRI is the technique of choice to exclude soft tissue extension as well as to detect intracranial meningioma as a potential site of metastatic spread [13]. Definitive diagnosis is given through suitable biopsy specimens. Immunohistochemical markers can be an important auxiliary tool in discerning it from other lesions [3, 7]. Intense reactivity for anti-EMA and vimentin are consistent with the diagnosis of meningioma [14]. S-100, claudin-1, glut-1 are important markers to discern meningioma from other lesions [7].
Meningiomas are usually divided into different histologic subtypes, such as meningotheliomatous, transitional, fibroblastic, psammomatous and angioblastic, according to the predominant cellular morphology. Excluding the angioblastic meningioma, which is a relatively aggressive variety, no significant biologic or prognostic differences have been found amongst the other histologic subtypes [3, 12, 14].
The therapy of choice for extracranial meningiomas in the jaws bones is surgical excision [1, 5, 10]. Kepes in 1982 states that the follow-up should be particularly close if a meningioma displays mitotic figures, invades bone or has foci of necrosis in it [9]. Undoubtful complete removal is still the most important factor in prevention of recurrence [9].
The prognosis of extracranial meningiomas after complete surgical tumour resection is good with disease-free rates of 82 and 78% at 5 and 10 years, respectively [10].
CONFIRMATION OF PATIENT’S PERMISSION
Informed consent was obtained from the patient who took part.
CONFLICT OF INTEREST STATEMENT
None declared.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.



