-
PDF
- Split View
-
Views
-
Cite
Cite
Gabrielle Yee, John D Hall, William R Hampton, Sai Yendamuri, Bo Xu, Elizabeth U Dexter, Massive hemoptysis resulting from a fistula between the bronchus intermedius and pulmonary artery: a novel clinical presentation, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa209, https://doi.org/10.1093/jscr/rjaa209
Close - Share Icon Share
Abstract
This is a case of a woman with massive hemoptysis, associated with a pulmonary artery pseudoaneurysm, and a fistula between the right pulmonary artery and bronchus intermedius. Bronchoscopic evaluation revealed an endobronchial mass in the right bronchus intermedius, suspicious for a tumor. Upon biopsy of the mass, massive bleeding occurred. The right lung was surgically resected. No specific etiology for the fistula was identified on pathologic examination. To our knowledge, this is the first report of a pulmonary artery-bronchial fistula presenting without typically known predisposing factors.
INTRODUCTION
A bronchovascular fistula associated with massive hemoptysis can be a devastating and potentially fatal condition that requires urgent intervention. Generally, blood loss over 1000 mL/24 h constitutes massive hemoptysis. Bronchovascular fistula associated with such life-threatening circumstances have been reported as a complication of multiple conditions. Lung interventions associated with fistula formation include endobronchial stent placement with erosion, anastomotic complications following pulmonary sleeve resection, lung transplantation and compromised bronchial stump after pneumonectomy. Some case series report that the incidence of bronchovascular fistulas can range from 2.6 to 13% [1, 2, 3, 4, 9]. However, the occurrence of such fistulas is rare in the absence of lung disease, specifically in the absence of invasive procedures.
CASE REPORT
The patient is a 53-year-old woman admitted following a 1-week history of increasing cough and shortness of breath. Her medical history includes type 2 diabetes, asthma, hypothyroidism, deep vein thrombosis (DVT’s), and methylenetetrahydrofolate reductase (MTHFR) gene mutation. Surgical history includes gastric bypass and Greenfield filter placement. Admission chest computed tomography angiography (CTA) was negative for pulmonary embolism (PE). There was peribronchial thickening and some bilateral ground glass changes suggestive of early pneumonia. The pneumonia was treated with ceftriaxone and azithromycin, along with systemic steroids and bronchodilators. She showed clinical improvement and was discharged uneventfully.
Initially, the patient reported feeling better, however, she then returned to the hospital 6 days later with worsening shortness of breath. Her course was now complicated with hemoptysis and hypoxia. The patient had been on rivaroxaban due to the history of DVT and thrombophilia. The oral anticoagulants were held on admission. A subsequent chest computed tomography demonstrated worsening right-sided pneumonia. There was also evidence of mild-to-moderate pneumopericardium and mild pneumomediastinum, due to small airway barotrauma from persistent coughing. There was a question of pseudoaneurysm of the right pulmonary artery which in retrospect appeared slightly enlarged from 12 days prior (Fig. 1a and b).
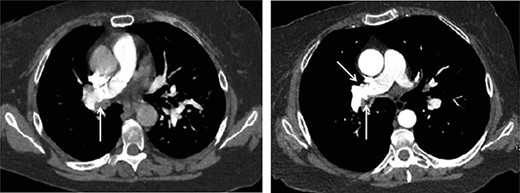
(1a) Axial CT chest slice shows small irregularity of right pulmonary artery wall (white arrow) with clot-filled bronchus. (1b) Axial CT chest slice shows increased irregularity of right pulmonary artery wall (white arrow) with open lumen bronchus. Possible opposite side pulmonary artery wall irregularity (yellow arrow).
On hospital Day 3, she developed massive hemoptysis with oxygen desaturation requiring emergent intubation. The patient was transfused with multiple units of packed red blood cells (PRBC’s) and fresh frozen plasma (FFP). She also required vasopressor therapy. Initial attempt at bronchoscopy was unsuccessful. Subsequently, the patient was transferred to another facility for a higher level of care.
Upon arrival the patient underwent bronchoscopy and placement of an endobronchial blocker via endotracheal tube. Clotted blood was seen filling the right main-stem bronchus with the tail of the clot noted along the medial wall of the left main-stem bronchus. Neither clot was disturbed at that time. She then underwent a pulmonary angiogram to evaluate for a possible coiling procedure for a presumed pulmonary artery pseudoaneurysm. However, no pseudoaneurysm or aberrant vessels were demonstrated on angiography (Fig. 2).

Pulmonary arteriogram with no visualization of right pulmonary artery wall irregularity.
Repeat bronchoscopy was done to evaluate the hemoptysis etiology. After carefully removing residual clot on the right side, an endobronchial mass was seen in the distal bronchus intermedius, which was suspicious for a tumor (Fig. 3). During an attempted biopsy, the patient suffered an episode massive hemoptysis. The patient required transfusion of four units of PRBC’s and vasopressor support.
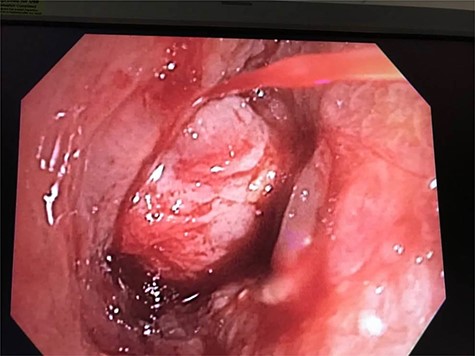
Bronchoscopic view of distal bronchus intermedius with surrounding inflammation and structure deceptive for endobronchial mass.
The patient was taken to the operating room for emergent thoracotomy. Bilobectomy was attempted but aborted because of dense inflammatory adhesions of the right hilum and bleeding with attempted dissection of the bronchus intermedius. A total right pneumonectomy was deemed necessary. Ex vivo dissection showed a fistula between the right pulmonary artery and the bronchus intermedius. Absence of malignancy or granulomatous disease was confirmed on final pathology. The patient had an uneventful postoperative recovery. She had no further episodes of hemoptysis.
Final pathology confirmed a pseudoaneurysm of the proximal pulmonary artery, lung parenchyma with extensive intra-alveolar hemorrhage, and bronchus intermedius with squamous metaplasia. No evidence of malignancy, granulomatous changes, cytopathic changes or capillaritis were noted in lung parenchyma. Lymph nodes were benign.
DISCUSSION
Massive hemoptysis is uncommon and very often fatal. We report a case of massive hemoptysis caused by a right pulmonary artery-bronchial fistula in a woman with no underlying lung disease, except for mild asthma. She had no previous thoracic procedures. To our knowledge, this is the first reported case of pulmonary artery-bronchial fistula associated with a pulmonary artery pseudoaneurysm. She is without underlying autoimmune disease such as Behcet’s disease, granulomatous disease with polyangiitis or fungal disease such as aspergillosis. There is no history of pulmonary embolism or pulmonary artery instrumentation. Extensive literature review revealed no known association between pulmonary pseudoaneurysm or bronchovascular fistula development, in relation to her other underlying medical conditions.
We do note a rarely reported case of massive hemoptysis from an idiopathic bronchovascular fistula. However, that case, unlike the case reported here, described a fistula between a segmental bronchus and a bronchial artery. The involved area was small enough to be treated with arterial embolization [5]. Our case, involved a much larger fistula and the presence of a pulmonary artery pseudoaneurysm.
Several articles report these types of fistulas as a complication in lung transplant recipients. This has been seen in patients transplanted for severe COPD [6], and pulmonary fibrosis [7]. Massive hemoptysis secondary to bronchovascular fistulas have been reported from 2 weeks to as far out as 4 years post lung surgery for malignancy [8, 9]. Bronchial-pulmonary artery fistulas have also been reported as complications of less invasive procedures such Swan-Ganz catheter insertion [10].
In each of these cases, possible causes of fistula formation appear related to instrumentation, or lingering inflammation of the pulmonary artery, causing vessel wall erosion. Poor anastomotic healing, ischemia of the airway, malignant tumors and opportunistic infections are contributing factors for bronchial-pulmonary artery fistula formation. No evidence malignancy, vascular malformation, granulomas, fungal or viral organisms, or capillaritis were identified in our patient.
To our knowledge, this is the first report of a pulmonary artery-bronchial fistula presenting without typically known predisposing factors. Interestingly, most of these reports including the present case, involve a right rather than left bronchial-pulmonary artery fistula. Whether or not there is anatomic predisposition to fistula formation on the right side rather than left has yet to be determined.
ETHICAL APPROVAL AND CONSENT TO PARTICIPATE
Consent has been obtained from the patient. Formal IRB review and approval is not required.
CONSENT FOR PUBLICATION
The patient and all authors have provided consent for publication.
DECLARATION OF CONFLICT OF INTEREST/COMPETING INTEREST
The authors declare no conflict of interest with respect to the research, authorship and/or publication of this article.
FUNDING
The authors have received no financial support for the research, authorship and/or publication of this article.
AUTHOR CONTRIBUTIONS
All of the authors contributed to patient care, case research, and/or preparation and critical review of the manuscript.
GUARANTOR/AVAILABILITY OF DATA AND MATERIALS
Elisabeth U. Dexter.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the contributions of Samad Rasul MD. His assistance in caring for this patient was invaluable.



