-
PDF
- Split View
-
Views
-
Cite
Cite
Stephanie Schwab, Christoph Kabbasch, Stefan J Grau, Spontaneous intraneural hematoma of the common fibular nerve due to oral anticoagulation, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa207, https://doi.org/10.1093/jscr/rjaa207
Close - Share Icon Share
Abstract
Compression syndromes affecting the common fibular nerve are common and frequently caused by direct pressure upon the fibular tip region. Here, we describe a case of a 50-year-old male presenting with sudden foot drop, which had developed spontaneously. He was on oral anticoagulants due to hereditary thrombophilia (factor-V-Leiden). Neurophysiology examination revealed a common peroneal nerve lesion at the fibular tip. T1-weighted magnetic resonance imaging (MRI) showed a not further classifiable hyperintensity within the common peroneal nerve. Surgical exploration revealed a diffuse intraneural hematoma, which was not evacuated. During follow-up, the nerve function recovered almost completely. In retrospect, MRI findings indicated a hematoma supported by the history of anticoagulant medication.
INTRODUCTION
The peroneal nerve is the most vulnerable neural structure of the lower extremity due to its superficial location close to the fibula. Common mechanisms of peroneal nerve injuries include traumatic traction or compression as well as entrapment syndromes caused by tumors or ganglion cysts. Medical history, electrophysiological assessment and imaging methods, comprising ultrasound and magnetic resonance imaging (MRI), are essential for obtaining the correct diagnosis and induction of treatment.
Here, we describe a spontaneous peroneal nerve palsy under anticoagulant medication with an otherwise uneventful history.
CASE DESCRIPTION
A 50-year-old male patient presented with a sudden and rapidly progressed right-sided foot drop and loss of sensation between the first and second right toe as well on the lateral thigh starting 3 days ago. After a mid-range flight to a professional appointment, he had noticed a painless weakness in the right foot during a meeting more than 6 hours after the flight. Due to previous pulmonary embolism resulting from a factor-V-Leiden mutation, he was on oral anticoagulants (phenprocoumon).
On clinical examination, the patient showed a weakness in dorsiflexion (Janda 3/5) and the great toe extension (0/5) as well as eversion weakness (3/5) on the right foot. A hypaesthesia was present in the corresponding area of the deep and superficial branch of the peroneal nerve with a positive Tinel’s sign in the area of the right fibula head. An MRI of the right knee and lower leg showed a discrete swelling of the common peroneal nerve and a slight hyperintense signal in T1-weighted images, which could not be further specified (Fig. 1). Motor nerve conduction studies showed a drop in amplitude across the fibular head and a slowed conduction velocity.
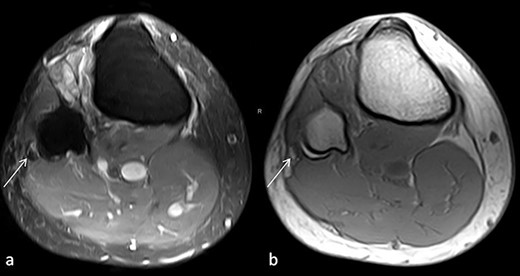
(a) Proton density, fat-saturated-weighted (PD FAT SAT) axial image: the arrow marks the swollen, hypointense peroneal nerve at the level of fibular head. (b) T1-weighted axial image: the arrow tags a hyperintense lesion in position of the peroneal nerve that may correspond to the intraneural haemorrhage.
Surgical exploration and decompression of the peroneal nerve revealed an intraneuronal hematoma of the common peroneal nerve (Fig. 2), which was not evacuated due to diffuse extension. Anticoagulant medication was paused perioperatively and restarted after 1 week. After the patient received intensive physiotherapy and electrostimulation, the nerve function showed good functional recovery to a degree of Janda 4+/5 within 4 months. A postoperative seroma had to be evacuated once with then proper wound healing.

Intraoperative photograph of the common peroneal nerve showing the hematoma (black discoloration).
DISCUSSION
Spontaneous symptomatic intraneural hematomas are rare but have been described for different nerves in patients with normal coagulation [1, 2]. Here, we report a first case of intraneural hematoma of the peroneal nerve in English literature. In our case, the patient was under oral anticoagulation since decades due to a hereditary thrombophilia and had not suffered from any complications so far.
The presumed pathomechanism at initial presentation was a pressure-associated nerval damage during the flight, although the patient stated convincingly that he had been walking for hours after the flight and had not noticed any difficulties. MRI imaging showed a somehow aberrant nerve signal at the fibular tip region, which could not be further classified by the neuroradiologist. Due to the high degree of motor impairment and an unclear lesion on MRI, we indicated an early surgical exploration and local decompression. Hematoma evacuation, as described in previous reports [2, 3], was not performed due to the absence of a defined clot but a rather diffuse extension throughout the nerve. Nevertheless, nerval function recovered well after conservative treatment.
In the literature, few cases of spontaneous intraneural hematomas are reported, most of them observed in the median nerve [2–4]. Richardson et al. presented two cases of hemorrhage in the sural and sciatic nerves, respectively [1, 2]. In most of these cases, an evacuation of the intraneural hematoma, including interfascicular neurolysis, was performed with good neurological outcomes [1–3, 5]. In our case, the hematoma spread diffusely throughout the nerve with no relevant thickening. Thus, no interfascicular preparation was made. However, functional recovery was good without a specific treatment for the nerve itself. While some experimental studies in rats showed better functional recovery and less axonal damage after evacuation of the intraneural hematomas [6, 7], in our case most probably surgery did not positively influence the natural course. In retrospect, MRI imaging was consistent with a small hematoma but was not characterized as such due to the rarity of intraneural bleeding. Retrospectively, surgery was probably redundant it both, neurosurgeon and neuroradiologist, had taken the possibility of a small hematoma due to anticoagulants into account.
CONCLUSION
Though being rare, this case may document an unusual event under oral anticoagulation therapy, which may be clarified by detailed MRI imaging and electrophysiological studies.
CONFLICT OF INTEREST STATEMENT
None of the authors has any conflict of interest to disclose.
FUNDING
None.



