-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammed Jihad Al Mahdi, Mohammed Asiri, Majed Pharaon, Ali Mubark, Frontal sinus inverted papilloma managed with Draf III, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa180, https://doi.org/10.1093/jscr/rjaa180
Close - Share Icon Share
Abstract
Inverted papilloma (IP) is a rare benign tumor that originates from nasal and paranasal sinus mucosa. Although it is considered a benign lesion, it is locally aggressive and has risk between 7 and 15% for malignant transformation. The management of frontal sinus (FS) IP is still challenging due to its rarity and local invasiveness. We report a rare case of IP originating from FS, and to review the literature to delineate the possible surgical strategy. A 52-year-old male presented with long-standing history of bilateral nasal obstruction and left eye proptosis. Sinus navigation computed tomography showed soft tissue density occupying frontal, ethmoid, right sphenoid sinuses with extension to nasal cavities, postnasal space and left orbital space plus erosive bony changes. Transnasal endoscopic biopsy suggested IP the lesion was completely resected by Draf III procedure. After 1 month of the surgery, the patient is doing well with no complaints.
INTRODUCTION
Inverted papilloma (IP) is a rare benign tumor that originates from Schneiderian mucosa of the nasal wall [1]. IP is a subtype of Schneiderian papillomas that also include exophytic and oncogenic papillomas [2]. The incidence rate of all sinonasal papillomas as per hospital-based studies is 0.74 per 100 000 residents per year [3]. Although IP is relatively uncommon, it is the most common type of Schneiderian papilloma, its rate among the sinonasal papilloma is 62% and it represents 0.5–4% of all nasal tumors [2]. Moreover, frontal sinus (FS) papilloma is very rare, it only represents 1–16% of the IP cases [4, 5]. For years, the management of choice for sinonasal papilloma was complete surgical resection via external approaches such as medial maxillectomy through lateral rhinotomy approach. But in the past 20 years the endoscopic approach has been evolved, and there are several evidence-based studies that have demonstrated the differences and the outcomes between the external and the endoscopic approaches [6, 7]. In this case report, we present a rare case of IP that originates from FS and has been managed endoscopically by Draf III approach.
CASE REPORT
A 52-year-old Saudi male presented in our outpatient clinic with a history of long-standing bilateral nasal obstruction with left eye protrusion for more than 1 year, which was associated with nasal discharge, hyposmia and headache. Past medical and surgical history was insignificant. No previous history of trauma or nasal surgery. Nasal examination with the aid of scope showed bilateral polypoid mass nearly obstruction nasal cavity.
Neck computed tomography (CT) scan performed first and showed expansile soft tissue lesion involving frontal and ethmoid sinuses extending to nasal cavity. There was associated left FS bony erosion and left orbital extension. Mild mucosal thickening of maxillary sinus is also noticed (Fig. 1).
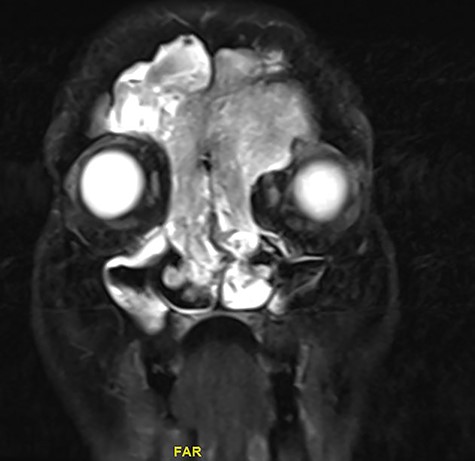
Magnetic resonance image (MRI) scanning also demonstrated a mass lesion involving both frontal and ethmoid sinuses, more into left FS causing expansion and rarefaction of the sinus wall, as well as extension of superior wall of left with extracoronal component causing mild proptosis. The lesion showed intermediate T2 signals with areas of high T2 signal along with postcontrast enhancement. No intracranial extension noticed (Figs 2 and 3).

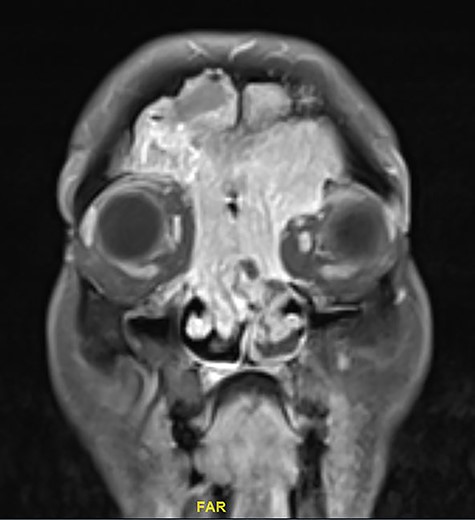
Coronal MRI of paranasal sinuses, T1-weighted image post contrast.
Based on neck CT and MRI features, the lesion most likely represent benign Sinonasal pathology mostly IP.
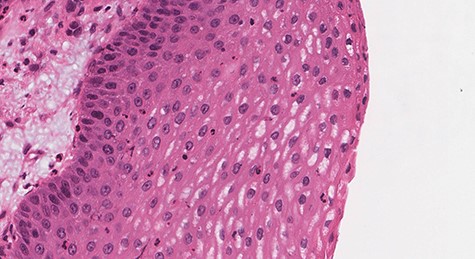
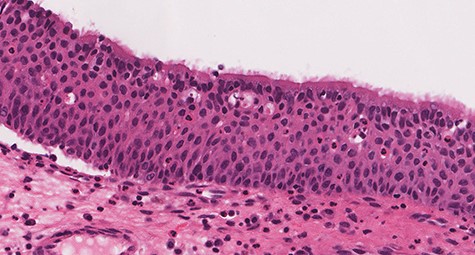
Biopsies obtained intraoperatively from the right FS, left FS and nasal cavity were consistent IP with no evidence of dysplasia or malignancy.
Histologic sections show an endophytic (inverted) pattern that grows downward into the underlying stroma (Fig. 4). The epithelium consists of hyperplastic squamous epithelium (Fig. 5) and ciliated columnar cells admixed with scattered mucocyets (goblet cells) (Fig. 6). The cells have a bland appearance and uniform small nuclei. No cytologic atypia, increased mitotic activity or necrosis seen. Mixed inflammatory cells are dispersed within the epithelium and stroma.
![Section of IP (hematoxylin and eosin [H&E] stain; ×29).](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2020/8/10.1093_jscr_rjaa180/1/m_rjaa180f4.jpeg?Expires=1771830741&Signature=GdSQQBo1uAERlxLkn7hrsIRxA58K9LI4khbqppI8-Soc19SkuJc60kMegKOblLRJUmYhrOjOEmpKuGByLTh-qDIB8M3gNGfWmxg9dl-~8XHbPLltVRprmU4eU-C-P74LdwZE5cYPhexMi0QkP37B5pxuo73cHw39goRL7b70wC6-Gfv8ZKFc3PKkR5aWML87SsoBlPiaxmzpeI5xbUImpb2G4~v5BFy6fy5Xu~0VcMnyKPYtw88GQFlLS0wwehgNtgAEbB1-4w2levt1TuynvTf-tv4fP8tRRnvllUfkwkNK3eLLR5IbfAU7B598WaAx5VEhJUFX0RLL9v4uBR2-MA__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
Debulking of the mass was done. Then, the nasal mass was removed from anterior and posterior ethmoid cells. We followed the mass to its origin, which was coming from the frontal recess and FS. The mass was debulked from the frontal recess on both sides. There was a defect in lamina papyracea on the left side with bulging over the left eye. Mass was removed from this bulging and removed slowly from the FS in both sides. A full Draf III surgery was done with removal of all tumor tissue. The postoperative course was uneventful; patient is doing well with resolution of nasal obstruction. He regularly visits the clinic for early detection of tumor recurrence.
DISCUSSION
The management of fontal sinus papilloma remains challenging due to its anatomical region and its invasive nature. The only treatment for IP is surgery. Moreover, there are multiple different surgical approaches, external and endoscopic approaches. Traditionally, the external approaches have been regarded as a standard of treatment. Furthermore, lateral rhinotomy with medial maxillectomy was the gold standard of the external approach. However, due to the advancement of imaging modality and the use of high-resolution CT and MRI prior and during the surgery, a more conservative management via endoscopic approach has been advocated by several authors. The endoscopic approach has remarkably improved. In addition, it has several advantages over the open approach as it gives better visualization around the lesions, better cosmetics and less postoperative hospital stay with few complications.
Tatwani T reported a case with IP in frontal recess. A frontal trephination was done through combined endoscopic-osteoplastic flap approach. Then, after 8 months of follow-up in outpatient clinic the patient presented with recurrent IP in FS, he was managed successfully with endoscopic Draf IIb. Then, the patient was followed for 1 year after the last surgery, with no signs or symptoms of recurrence [8].
A 25-year retrospective analysis of the endoscopic management results in 29 patients presented by Sham et al. [9] suggests that the operative strategy should be selected based on the location of tumor origin in patient. The locations were categorized into following five groups: F1, tumor prolapsed into FS, tumor origin outside FS; F2, tumor origin inside FS, medial to the plane of lamina papyracea; F3, tumor origin inside FS, lateral to the plane of lamina papyracea; F4, bilateral; and F5, extrasinonasal. And concluded that Draf I or IIA surgery is adequate for most F1 tumors, and Draf II surgery is adequate for most F2 tumors. F3 and F4 tumors can be managed initially by Draf III surgery with external frontal sinusotomy added when required. F5 tumors probably require combined surgical approaches [9].
CONCLUSION
FS IP is a rare entity. It is characterized by its local destruction, high rate of recurrence and risk of malignant transformation. Imaging and biopsy aid in diagnosis. The endoscopic approach is now the gold standard. Combined approach is reserved for selected cases. Draft III FS surgery can be enough in selected patients with FS IP.



