-
PDF
- Split View
-
Views
-
Cite
Cite
Masayo Kawakami, Hidetsugu Nakazato, Takeshi Tomiyama, Takehiko Tomori, Jun Miyagi, Seiji Nagayoshi, Yasushi Ohmine, Laparoscopic sigmoidectomy for sigmoid colon cancer with left-sided inferior vena cava and persistent descending mesocolon, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa259, https://doi.org/10.1093/jscr/rjaa259
Close - Share Icon Share
Abstract
Left-sided inferior vena cava (IVC) is a rare congenital malformation, as is persistent descending mesocolon, a developmental anomaly in which the colonic mesentery does not fuse with the dorsal abdominal wall. Although these anomalies are mostly asymptomatic, they should be identified preoperatively to avoid iatrogenic injury. We report a case of sigmoid colon cancer in a patient with both anomalies. The patient was an 80-year-old man whose preoperative computed tomography (CT) scan showed that the IVC ascended vertically along the left side of the abdominal aorta, and the descending colon was at the abdominal midline. Coronal CT was particularly useful for visualizing these anomalies. With this better understanding of the malpositioned anatomy, we successfully performed laparoscopic sigmoidectomy with lymph node dissection. Careful evaluation of preoperative CT imaging based on a clear understanding of such anatomical anomalies is particularly important for performing safe laparoscopic surgery.
INTRODUCTION
Left-sided inferior vena cava (IVC) is a rare congenital anomaly with a reported worldwide incidence of 0.2–0.5% [1]. Although this anomaly is usually found incidentally on imaging studies performed for other reasons, it becomes clinically significant in patients who require retroperitoneal surgery.
Persistent descending mesocolon (PDM), also a rare congenital anomaly, results from failure of fusion between the primitive dorsal mesocolon and parietal peritoneum during the fifth month of gestation [2]. Although it is asymptomatic in most cases, some clinical complications have been associated with PDM (such as, colonic volvulus and intussusception) [3,4]. With respect to abdominal surgery, one must be aware that unusual mesenteric adhesion or arterial abnormalities have been associated with PDM [5]. Thus, preoperative diagnosis of such anomalies and careful surgical procedures are important. We report a rare case of sigmoid colon cancer in a patient with left-sided IVC and PDM. He was treated with laparoscopic surgery.
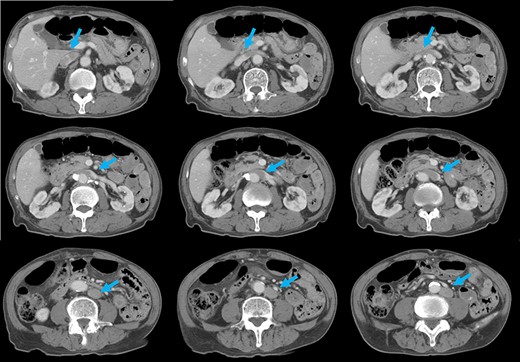
CT shows that, after connecting with the left renal veins, the left-sided IVC (arrows) crosses the abdominal aorta anteriorly to join a normal prehepatic segment of the IVC.
CASE REPORT
An 80-year-old Japanese man with no significant medical history presented to another clinic with dizziness. Blood tests revealed severe anemia. Later, at our institution, he underwent intestinal endoscopy, which revealed a mass in the sigmoid colon. Histological findings of the biopsy specimen indicated colon cancer.
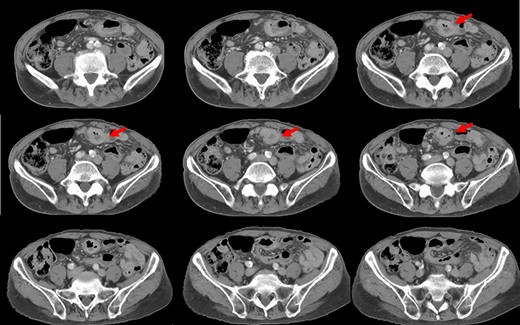
Preoperative computed tomography (CT) revealed a tumor in the sigmoid colon accompanied by some regional lymph node swelling (Fig. 1). It also showed that the IVC ascended vertically along the left side of the abdominal aorta. After connecting with the left renal veins, the left-sided IVC crossed the abdominal aorta anteriorly to join the normal prehepatic segment of the IVC (Figs 2 and 3). Coronal CT showed that the descending colon misplaced at the abdominal midline and the sigmoid colon in the right upper abdomen (Fig. 4). The preoperative diagnosis was thus sigmoid colon cancer with left-sided IVC and PDM.
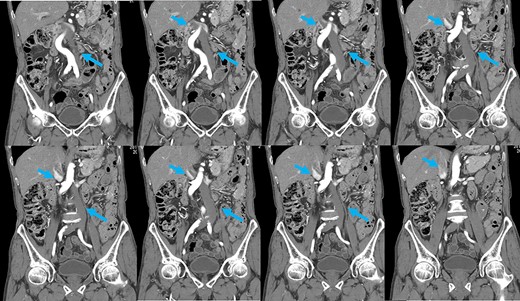
Coronal reformation of the CT image shows precisely how the left-sided IVC (arrows) ascended vertically along the left side of the abdominal aorta and crossed anterior to the aorta.
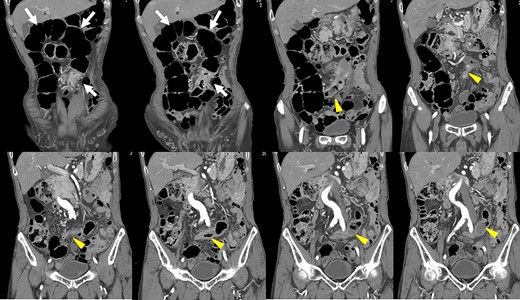
After coronal reformation, the CT images show that the descending colon was at the midline of the abdomen (arrowheads), and the sigmoid colon was in the right upper abdomen (arrows).
Laparoscopic sigmoidectomy with left colic artery-preserving D3 lymph node dissection was performed using a five-port technique. At an early stage of the operation, the sigmoid colon and sigmoid mesocolon were found adherent to the ileum and right side of the abdominal wall. Furthermore, the descending colon was not fixed to the retroperitoneum and had shifted to the midline of the abdomen (Fig. 5a and b). After separating this abnormal adhesion, the sigmoid mesocolon was mobilized in a mediolateral fashion while paying close attention to preserving the peritoneal layer covering the hypogastric nerves (Fig. 5c). Because the left-sided IVC was just below the peritoneum, it could be seen through the thin peritoneal layer together with the retroperitoneal structures (including the left ureter and left gonadal vessels) (Fig. 5d). After resecting the sigmoid colon, a functional end-to-end anastomosis was performed using a linear stapler.
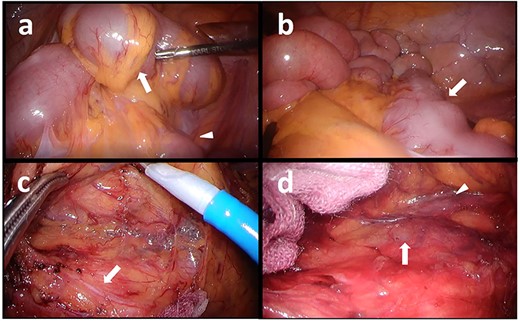
Intraoperative images: (a) Adhesion between the sigmoid colon (arrow) and the ileum (arrowhead), (b) The descending colon (arrow), (c) Dissection plane (hypogastric nerve is shown by the arrow), and (d) The left-sided IVC (arrow) and the left ureter (arrowhead).
The patient’s postoperative course was uneventful, and he was discharged 10 days after the operation.
DISCUSSION
Formation of the IVC is a complex process involving the development, regression, anastomosis and replacement of three pairs of main embryonic veins [6,7]. In the order of their appearance, they are the posterior cardinal, subcardinal and supracardinal veins. The error in the formation process may result in four IVC anomalies: IVC duplication, transposition resulting in a left-sided IVC, retroaortic left renal vein and circumaortic left renal vein [8]. Left-sided IVC results from regression of the right supracardinal vein with persistence of the left supracardinal vein. Typically, the left-sided IVC ends at the level of the left renal vein, where it crosses anterior to the aorta to form a normal right-sided IVC [1].
Most left-sided IVCs are asymptomatic, although patients with IVC malformations are at significant risk of developing a deep vein thrombosis [9]. When a left-sided IVC is encountered, the patient must be evaluated for a possible thrombosis. The main clinical significance of left-sided IVC is the associated risk of iatrogenic injury during retroperitoneal surgery because it may be diagnosed as para-aortic lymphadenopathy, a tumor or a dilated gonadal vein. Regarding patients undergoing laparoscopic sigmoidectomy, fatal IVC damage is possible if the sigmoid mesocolon is mobilized in the deeper stripping layer. Accurate preoperative evaluation of the retroperitoneal caval system anatomy and meticulous dissection with a correct layer may permit a successful laparoscopic approach.
PDM is a developmental anomaly characterized by failure of the descending mesocolon mesentery to fuse with the posterolateral parietal peritoneum [2]. The non-fused mesentery is then responsible for considerable variations in the position of the descending mesocolon. In our case, the descending colon was at the abdominal midline, and the sigmoid colon was in the right upper abdomen. Coronal reformatted images obtained by multidetector CT (MDCT) proved useful for an accurate preoperative diagnosis of the malpositioned descending colon. It is widely accepted that MDCT is an effective technique for staging colon cancer preoperatively [10]. MDCT also allowed us to generate multiplanar coronal images, which depicted the location of the colon as it would appear during the surgery. Moreover, MDCT angiography can be used to evaluate the running direction of the vessels. Because it has been reported that the left colon and sigmoid colon arteries and the superior rectal artery often branch radially from the inferior mesenteric artery, and that a marginal vessel may run abnormally due to the unusual mesenteric adhesion [5], accurate evaluation of the arteries is important for safe lymph node dissection.
To the best of our knowledge, there have been no other reports of sigmoid colon cancer coexisting with left-sided IVC and PDM. Careful evaluation using preoperative CT imaging based on understanding these anatomical anomalies may allow safe performance of laparoscopic surgery.
CONFLICT OF INTEREST STATEMENT
None declared.
ACKNOWLEDGMENT
We thank Nancy Schatken, BS, MT(ASCP), from Edanz Group (https://en-author-services.edanzgroup.com/), for editing a draft of this manuscript.
References
- congenital abnormality
- computed tomography
- abdominal aorta
- laparoscopy
- mesentery
- mesocolon
- preoperative care
- inferior vena cava
- abdomen
- colon
- diagnostic imaging
- lymph node dissection
- persistence
- laparoscopic surgery
- abdominal wall
- iatrogenic injuries
- colectomy, sigmoid
- descending colon
- sigmoid cancer



