-
PDF
- Split View
-
Views
-
Cite
Cite
Miguel A Moyón, Gabriel A Molina, Braulio Aaron Crisanto, F Xavier Moyón, Andrés Cárdenas, Ricardo A Buenaño, Santiago E Gallegos, Sindy Mishel Espinoza, Duodenal perforation after percutaneous fluid drainage, a rare event: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa206, https://doi.org/10.1093/jscr/rjaa206
Close - Share Icon Share
Abstract
Duodenal perforations can be caused by surgical instruments during operations. These injuries can go initially unnoticed and lead to problematic complications. While uncommon, bowel perforation after percutaneous fluid drainage can severely impact the patient’s outcome. These can occur from equipment used for image-guided percutaneous drainage, a technique that has changed the way surgeons handle postoperative fluid collections and has become daily practice. Prompt recognition and timely treatment of these types of complications can minimize the consequences of this dreaded scenario. We present the case of a 29-year-old male, for whom an intra-abdominal collection was detected after laparoscopic cholecystectomy. CT-guided percutaneous drainage was performed, during which the catheter inadvertently punctured the duodenum. Surgical consultation was required and, since the patient remained asymptomatic, conservative management of the duodenal perforation was accomplished without complications. On follow-ups, the patient is doing well.
INTRODUCTION
Postoperative fluid collection and abscess management have improved in recent years due to the development of image-guided drainage techniques, a medical procedure generally considered safe but where complications are still expected to happen on occasion. Duodenal perforations following minimally invasive procedures are rare, yet they can have troublesome complications when they occur [1, 2].

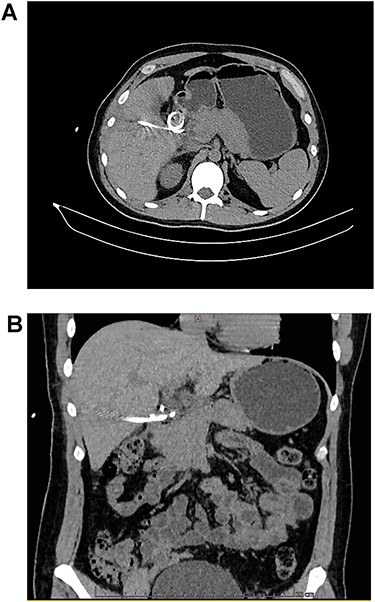
A: CT, the catheter tip can be seen lodged in the duodenal lumen. B: CT, the catheter perforates the duodenal wall.
We present the case of a 29-year-old male with past medical history of laparoscopic cholecystectomy. An intra-abdominal collection was detected after surgery and CT-guided percutaneous drainage was performed. The catheter inadvertently punctured the duodenum and its tip lodged inside its lumen. Conservative management of the duodenal perforation was completed without complications. On follow-up, the patient is doing well.
CASE REPORT
The patient is a 29-year-old male, without past medical history. He was admitted to a private clinic due to acute cholecystitis 1 month prior. After said surgery, he was discharged on his second postoperative day without any apparent complications. Nonetheless, eight days after surgery, he experienced high fever and diffuse abdominal pain, and presented back to said clinic. A contrast-enhanced computed tomography (CT) revealed a low-density intra-abdominal collection of 105 cc (density = 25 Hounsfield Units) filled with gas. Broad-spectrum antibiotics were initiated and percutaneous drainage of the intra-abdominal collection was decided. A CT-guided percutaneous drainage was completed using a 12 French pigtail catheter, from which 100 cc of purulent fluid was recovered. A multisensitive Escherichia coli isolate was cultured from the sample. During the following five days after the drainage procedure, the output of the drain remained low and serous (15–20 mL/day). Nonetheless, on the sixth day after the procedure, the output increased (300–400 mL) and the fluid became bilious. Intestinal or biliary fistulas were among the differentials, and a new CT was planned. However, the patient requested his discharge against medical advice (due to the increasing costs associated with the treatment) and presented to our hospital, a publicly funded institution, 12 hours later. On arrival, the patient was asymptomatic, reported no changes in bowel functions or discomfort while eating and presented no febrile episodes. His clinical examination was unremarkable and the catheter drained bilious content (Fig. 1). Complementary exams including a complete blood count revealed normal leukocytes (7.5 × 109) without neutrophilia (45%), and electrolytes were also under normal, expected ranges. Thus, a new contrast-enhanced CT revealed that the pigtail catheter perforated the lateral wall of the second portion of the duodenum, with its tip lodging inside the intestinal lumen (Fig. 2A and B).
A fistulogram using the catheter was completed, which confirmed our diagnosis. As the patient remained in good condition and asymptomatic, the duodenal perforation was considered contained and conservative management was decided (Fig. 3). Total parental nutrition and NPO (nil per os) were started and the output of the drain dramatically diminished. On the 10th after the diagnosis, the catheter was removed without complications, as the daily output of the drainage did not exceed 50 cc. Sips of clear liquids were initiated immediately, followed by a full diet with no difficulties. He remained completely asymptomatic and was discharged on his 15th day. On follow-up consultations 3 months after the drainage procedure, patient is doing well.

CT reconstruction, the contrast is spreading to the duodenum and small bowel without leaks.
DISCUSSION
Duodenal perforation is a rare but dangerous complication with a high mortality rate ranging between 8 and 25% [1]. Through the widespread use of protein pump inhibitors and the combined treatment of Helicobacter pylori, duodenal perforations due to peptic ulcers are now unusual [1, 2], but occurrence of these injuries caused by trauma and iatrogenic duodenal perforations can still occur [1]. Since the late 1970s, image-guided percutaneous drainage has changed the traditional surgical approach for intra-abdominal collections and abscess with excellent results (up to 80% success rate) [2]. Nonetheless, like any medical procedure, complications such as infections, bleeding and fistula formation can occur [2]. While the incidence of bowel perforations during percutaneous drainage is less than 1% [2], inadvertent catheterization or perforation of the intestines, liver, spleen or stomach has been reported [2]. When the bowel is punctuated with a small needle (21-G), the vast majority of cases will show no symptomatology or complications [2, 3]. Nonetheless, when wider catheters puncture the bowel wall, intestinal fluid can be observed in the drainage [2, 3]. This can happen several days after the initial injury to the intestinal wall, or even at later times [3]. We believe that a duodenal puncture occurred during the previous procedure that our patient was submitted to, which only became apparent after a few days.
When a drain inadvertently punctures the duodenum, an external duodenal fistula can appear that can lead to the interruption of the intestinal continuity and leading to loss of intestinal contents, electrolyte disorders, sepsis and even death [1, 4, 5]. However, conservative management of duodenal injuries can be appropriate and successful if peritoneal signs are not present [1, 4, 5]. Bowel rest, supportive care, and withdrawal of the catheter without any surgery is possible if there is a mature tract developed, which can be confirmed through a fistulography with contrast [4]. This approach proved effective for our patient. If signs of peritonitis develop, urgent surgery is usually necessary [1, 3, 5], a course of action avoided in our case as the patient was completely asymptomatic. There are various reports of duodenum puncture during percutaneous nephrolithotomy or endoscopic treatments that were managed similarly to our case, with conservative therapy [6, 7].
Percutaneous fluid drainage is a routine procedure and, like any medical interventions, can present occasional complications. When these arise, the decision of the medical team will directly impact the outcome of the patient, emphasizing the importance of adequate clinical management and technical capacity If a complication after percutaneous drainage is suspected, prompt diagnosis and treatment are vital to overcome these rare but critical scenarios.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conf lict of interest.
Funding
None.



