-
PDF
- Split View
-
Views
-
Cite
Cite
Alexia Grech, Naomi Mercieca, Jean Calleja-Agius, Rachel Abela, Metastatic malignant melanoma of unknown primary in temporalis muscle, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa202, https://doi.org/10.1093/jscr/rjaa202
Close - Share Icon Share
Abstract
Metastatic melanoma of unknown primary (MUP) is an uncommon melanocytic lesion found in distant sites with no evident skin involvement. This case report presents a 75-year-old woman who underwent local excision for a lump in the right temporal area, which had been present for 6 months and had been suspected to be a lipoma. Histology confirmed that the tissue excised from the temporalis muscle was composed of atypical, heavily pigmented melanocytes. Her history was negative for melanocytic lesions, and examination and extensive investigation including imaging had failed to identify a primary lesion. The patient is currently being followed up.
INTRODUCTION
Malignant melanoma is the commonest skin tumour worldwide, although it is known to occur in other organs, and its incidence is on the rise [1]. Metastatic melanoma of unknown primary (MUP) is a melanocytic lesion in distant sites in the absence of apparent skin involvement and is rare, accounting for up to 6% of all incident melanomas [2] as well as being yet poorly understood in terms of pathogenesis.
CASE PRESENTATION
A 75-year-old woman presented to a surgical outpatients clinic with a 6-month history of a lump in the right temporal area, occasionally tender and slowly increasing in size. She denied any hearing or visual symptoms and had no previous history of malignant melanoma or the presence of any melanocytic skin lesion. However, she reported an episode of trauma to the right temporal area ~6 months previously. She is hypertensive, asthmatic and an ex-smoker.
On examination, the patient had a 4-cm non-tender slightly fluctuant non-pulsatile mass over the right temporal area, clinically suggestive of a lipoma. On examination, there were no melanocytic naevi on the overlying and surrounding skin, and fundoscopy was normal. Blood investigations were within normal limits, except for thyroid function tests, which were suggestive of hypothyroidism. Computed tomography (CT) imaging of the head, neck and thorax demonstrated a 2 × 4 x 4 cm well-defined subcutaneous enhancing soft tissue formation in the right temporal fossa (Fig. 1). There was no cervical lymphadenopathy and no lung consolidation or suspicious lung nodules.
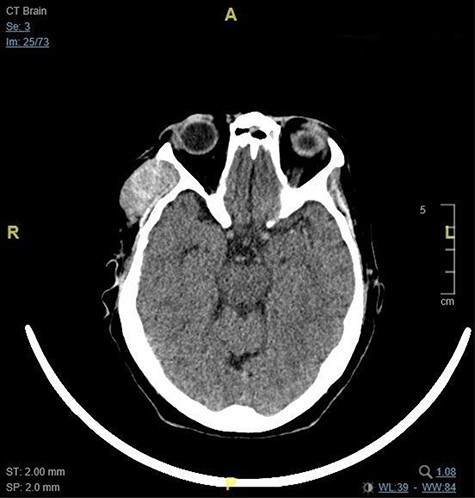
This image shows the 2 x 4 x 4 cm right temporal fossa lesion as seen on CT brain in the axial plane.
At excision of the lesion under local anaesthesia, a collection of dark semi-solid material within the temporalis muscle, resembling a haematoma, was noted and sent for histological analysis. She underwent primary closure of the wound, with intraoperative insertion of a drain that was removed the following day prior to discharge.
The patient was followed up at the surgical outpatients clinic (Fig. 2). Histology confirmed that the tissue was composed of atypical, heavily pigmented melanocytes and was negative for BRAFV600 mutation (Fig. 3). She was referred for review by an oncologist and a dermatologist. A positron emission tomography–computed tomography (PET–CT) scan showed a sizeable focus of abnormal increased uptake in the right temporalis region with no other evidence of abnormal tracer accumulation. She was later started on nivolumab for Stage 4 melanoma, but within 4 months was noted to have developed local progression of disease and new liver metastasis on a follow-up PET–CT scan. She is currently being managed palliatively.

This image shows the post-operative scar in the right temporal region.
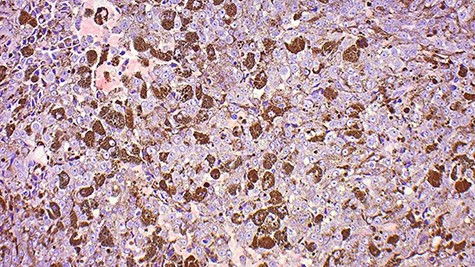
This image shows a tumour comprised of neoplastic epithelioid cells with prominent central nucleoli, most of which feature cytoplasmic melanin.
DISCUSSION
Malignant melanoma is an aggressive tumour of melanocytes, which are derivatives of the neural crest cells [1], and its common presentations as cutaneous, mucosal or ocular lesions allow for its classification [3]. MUP is defined as a histologically confirmed melanoma found in skin, subcutaneous or visceral tissues or lymph nodes, with no manifestation of a primary lesion [3]. MUPs comprise up to 6% of diagnosed melanomas, 60% of which are present in lymph nodes, and reports of intramuscular lesions as in this case are rare [3]. To our knowledge, this is only the fourth such report [3–5]; as in Mercer and Deveraj’s [4] case, a diagnosis was reached upon excision and investigation failed to identify a primary.
The pathogenesis for MUP is not well understood; however, potential aetiology includes the spontaneous regression of a previously unrecognized primary melanoma [6] after metastatic spread [7] or a previous melanoma that was removed as a result of trauma or excised with no [6] or an incorrect pathological diagnosis [7]. The presence of concurrent clinical unrecognized melanoma or de novo malignant transformation of an ectopic melanocyte at a visceral site or lymph node have also been proposed as causing MUP [2]. Lee et al. [6] propose that MUP is most likely a result of immune-induced regression of the primary tumour. This is because increased CD3 T-lymphocytes and elevated expression of the interleukin 2 receptor (which marks activated T-cells) have been identified in regressing primary melanomas in response to the presence of melanoma-associated antigens [8]. Humoral mechanisms for regression have also been suggested after identification of antibodies on melanocyte cell membranes by immunofluorescence [6] and following correlation of the endogenous immune response with improved survival. It is likely that regression might involve a combination of both humoral and cellular immune responses [6].
The predominant mutation linked with melanoma (80–90% of cutaneous primary melanoma) is the BRAF mutation type V600E, which has been associated with shorter survival [9], and a similar mutation profile between cutaneous primary melanoma and MUP has been observed [7]. However, in patients with MUP, BRAF mutation status does not appear to have a significant impact on prognosis [7].
The 5-year overall survival rates of patients with MUP are reported to range between 28.6 and 75.6% in patients who present with lymph node disease and from 5.9 to 18% in patients who present with visceral disease [10]. Furthermore, patients with MUP and lymph node disease have similar or better survival in comparison with stage-matched patients with melanoma of known primary. Treatment depends upon the staging of the lesion and can range from surgical excision to oncological treatment with radiotherapy and chemotherapy [3] but should be the same as that for stage-matched patients with melanoma of known primary.
CONCLUSION
This case report illustrates the necessity of more research into the pathogenesis and management of MUP, an unusual lesion for which diagnosis is crucial to the clinical care of a patient. With involvement of a multidisciplinary team for prompt diagnosis, complete staging, adequate treatment and close follow-up, the prognosis of patients with MUP can be improved.
CONFLICT OF INTEREST STATEMENT
None declared.



