-
PDF
- Split View
-
Views
-
Cite
Cite
Mariangela Mancini, Nicolò Leone, Massimo Iafrate, Ambrogio Fassina, Filiberto Zattoni, in collaboration with European Reference Network for Rare Urogenital Diseases and Complex Conditions (ERN eUROGEN), Spontaneous intra-adrenal massive hematoma: possible extreme evolution of a non-secreting untreated adrenal adenoma, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa185, https://doi.org/10.1093/jscr/rjaa185
Close - Share Icon Share
Abstract
The spontaneous adrenal hematoma is a rare event. An 83-year-old male patient presented a 26-cm asymptomatic retroperitoneal mass of doubtful renal–adrenal origin. He had been evaluated 10 years before for an adrenal incidentaloma of 2.3 cm and had refused surgery when it had reached 7 cm. Later, the mass enlarged to 26 cm and was surgically removed through an open anterior approach. The histopathology showed a solid 4 kg mass of fibrinoid–hemorrhagic material, partially necrotic, mixed with adrenal tissue, with a well-vascularized capsule. No relapse is present at 6-month follow-up. This is the largest case described of spontaneous intra-adrenal hematoma in a case with previous non-secreting adrenal adenoma. The hematoma (a 4 kg mass) developed 10 years after the first diagnosis and exposed the patient to potential damage of the surrounding organs and to high-risk abdominal surgery. Long-term follow-up of non-secreting adrenal adenomas should be recommended.
INTRODUCTION
The adrenal incidentaloma is an asymptomatic mass detected by chance on imaging, of different nature, including benign and malignant lesions. The most frequent tumor types are non-functioning cortical adenomas; less frequent are functioning lesions of the cortex, pheochromocytomas, adrenal carcinomas, myelolipomas, metastases and cysts [1]. In total, 15 cases of spontaneous adrenal hematoma have been reported in patients with or without history of adrenal tumor, with a maximum diameter of 7 cm [2].
CASE REPORT
An 83-year-old male patient with no history of hypocoagulative conditions or anticoagulant medications, presented to the hospital after a right thoracic trauma, and was hospitalized for right hemothorax and fracture of the omolateral VII–X ribs. On physical examination, a mass on the left upper abdominal quadrant was incidentally noted. An additional thoracic–abdominal contrast computed tomography (CT) scan documented a left retroperitoneal mass of doubtful renal–adrenal origin, displacing the spleen, the body–tail of the pancreas, the left kidney and the stomach (Fig. 1a and b). No signs of metastatic disease were present.
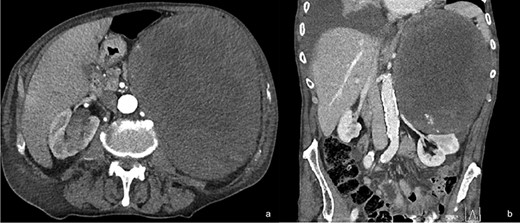
Contrast CT scan of the abdomen of the patient at his admission in the hospital. Axial view showing a left abdominal mass occupying the left upper abdominal quadrant and displacing down the left kidney (a) and renal artery and vein as shown in the coronal view (b).
The patient reported a previous history of left non-secreting adrenal incidentaloma, diagnosed 10 years before. At the time of diagnosis, the tumor diameter was 2.3 cm, with CT densitometry suggestive for benign adenoma (Fig. 2); the patient had been invited to regular follow-up visits, which he never attended. After 6 years, a new contrast CT demonstrated a growth of the tumor up to 7 cm. The clinical examination had excluded symptoms and signs of adrenal hormonal excess. A new complete evaluation of the endocrine situation was repeated: 1 mg overnight dexamethasone suppression test excluded cortisol excess; pheochromocytoma was excluded by the measurement of urinary fractionated metanephrines; because the patient was hypertensive, aldosterone/renin ratio was performed after 2-month washout from interferent antihypertensive drugs and a primary aldosteronism was excluded; all other laboratory tests were regular. The patient was asymptomatic and decided to discontinue his follow-up, coming back to medical attention the day of the trauma. After treatment of the hemothorax, the patient recovered completely and was discharged. Subsequently, he was submitted to abdominal open surgery through an anterior approach. A Chevron bilateral subcostal incision was made; the left colon mobilized, with careful dissection of the mesocolon from the mass. The left retroperitoneal space was accessed, displaying an imposing vascularized mass occupying the upper left abdomen (Fig. 3a–d). The mass displaced the left kidney, determining a verticalization downward of the left renal artery and vein and was in close contact with the upper pole of the kidney without having clear cleavage plans (Fig. 1b). On the other hand, the splenic artery and vein were displaced vertically upward. Careful dissection of the mass allowed its complete removal without damaging the surrounding organs and vessels, with ligation of the adrenal vein (Fig. 3d), as well as large lumbar vessels vascularizing the mass. Blood loss was 2500 cc, and the patient was transfused with 5 units of concentrated red blood cells. Final dimensions of the mass on the operating table were 26 × 21 × 12 cm, weight = 4.5 kg (Fig. 4). Two abdominal drains were left in place and removed on the fourth and fifth postoperative day. The postoperative clinical course was uneventful, and the patient was discharged on the seventh postoperative day without complications. At 6-month follow-up visit, the patient presented no symptoms and no signs of recurrence.
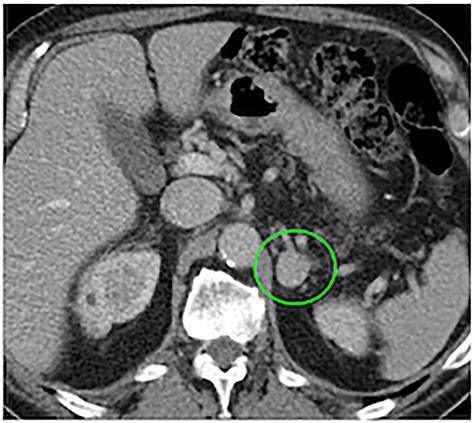
Ten years before abdominal CT scan, provided by the patient, at the time of first diagnosis, showing a 2.3-cm mass at the level of the left adrenal gland (green circle).
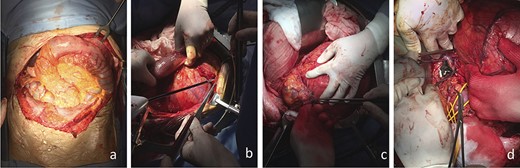
Surgical images, (a) subcostal bilateral incision showing the large retroperitoneal mass growing behind the transverse mesocolon and the left colic flexure; (b) careful isolation of the mass from the surrounding organs; (c) identification and preservation of the left upper pole of the kidney; (d) ligation of a large left adrenal vein joining the left renal vein displaced vertically downward.

Final image of the mass on the operating table after removal, with its complete capsule.
Histopathological examination showed sections of adrenal gland with large areas substituted by thrombosed fibro-hemorrhagic material surrounded by a richly vascularized fibrous capsule. The final histological diagnosis was ‘organized and partially revascularized long-term intra-adrenal hematoma’. At light microscopy (Fig. 5), the mass was composed of large hemorrhagic lacunae filled with fluid blood or organized in small or large thrombi (Fig. 5c). The larger thrombotic formations were revascularized with evident proliferating endothelial cells in the new vessels (Fig. 5f). The mass was well contained within the adrenal capsule, which appears collagenized and thicker than usual, often containing residual adrenal tissue (Fig. 5a and b), mostly from the granulosa layer. The problem of differential diagnosis with an angiosarcoma was ruled out by the absence of atypical endothelial nuclei, absence of mitotic figures and the limited necrotic areas. CD31 (Fig. 5d), the vascular cell adhesion and signaling molecule, PECAM-1, in endothelial cells, was strongly positive, demonstrating the restored vascular permeability barrier following disruption of the endothelial cell junctions [3], as well as FLI-1 (Fig. 5e), a valuable marker of endothelial differentiation [4].
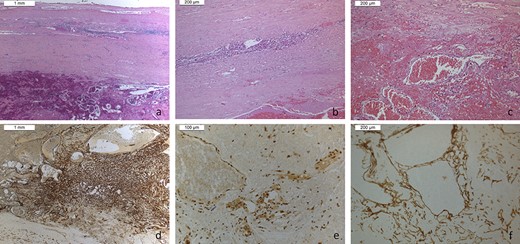
Hematoxylin–eosin sections (a–c) and differential immunohistochemistry (CD31, FLI1, Podoplanin) sections, excluding malignant vascular growth or sarcomas (d–f).
DISCUSSION
A spontaneous intra-adrenal hematoma in patients with no history of abdominal surgery and no hypocoagulative conditions has been reported a few times, and <5 times in patients with history of adrenal adenoma [2, 5].
The European Guidelines for adrenal incidentalomas indicate open adrenalectomy in case of unilateral adrenal masses with radiological findings suspicious of malignancy and signs of local invasion; laparoscopic adrenalectomy is indicated in case of masses < 6 cm without signs of local invasion. The adrenalectomy is also advised in case of a size increase of >20% in 6-month follow-up [1]. In our case, there were elements suspicious of malignancy (large contrast-enhanced growing mass, with signs of local invasion of the kidney). The histological report described a benign condition such as a massive spontaneous hematoma of the left adrenal gland. Some authors suggest performing magnetic resonance imaging with gadolinium-diethylenetriamine pentaacetic acid dynamic perfusion study to allow better characterization of adrenal hematomas to avoid surgery for smaller hematomas [6].
In conclusion, the spontaneous adrenal hematoma is a rare condition to be considered in the differential diagnosis of cases of adrenal non-functioning growing masses, especially in asymptomatic patients. The spontaneous hematomas reported so far were <7 cm. We report a case of incidental finding of a 26-cm spontaneous intra-adrenal hematoma in a patient with history of non-secreting adrenal adenoma, who had discontinued voluntarily his follow-up. This case represents a possible evolution of a small non-secreting adrenal adenoma, which had shown initial growth after 10 years from the first diagnosis and developed slowly into a 4 kg retroperitoneal mass, exposing the patient to potential damage of the surrounding organs and high-risk abdominal surgery.
CONFLICTS OF INTEREST STATEMENT
None declared.
ETHICS APPROVAL
Ethical approval was waived by the local ethics committee at the University of Padova, in view of the retrospective nature of the study, and all the procedures being performed were part of the routine care.
CONSENT TO PARTICIPATE
The patient has consented to the preparation of the case report for submission to the journal.
CONSENT TO PUBLICATION
The patient has consented to the submission of the case report to the journal and has signed informed consent for publication of all the images in the figures.
AUTHORS’ CONTRIBUTIONS
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by M.M. and N.L. The first draft of the manuscript was written by M.M. and N.L. All authors commented and critically reviewed previous versions of the manuscript. All authors read and approved the final manuscript.



