-
PDF
- Split View
-
Views
-
Cite
Cite
Abhijeet Kumar, Ratish Karn, Bhawani Khanal, Suresh Prasad Sah, Rakesh Gupta, Laparoscopic approach for diaphragmatic hernia repair in adult: our experience of four cases, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa178, https://doi.org/10.1093/jscr/rjaa178
Close - Share Icon Share
Abstract
Diaphragmatic hernia can be congenital or acquired. Usual clinical presentation may range from asymptomatic cases to serious respiratory/gastrointestinal symptoms and occasionally atypical presentation as lumbar hernia also. The diagnosis of diaphragmatic hernia is based on clinical investigation and is confirmed by plain X-ray film and computed tomography scan. Various treatment approaches, open, laparoscopic and combination, are available for this condition. However, laparoscopic approach has recently gained in popularity. Surgical repair typically involves primary or patch closure of the diaphragm through an open or endoscopic abdominal or thoracic approach. This paper reflects our experience of repair of diaphragmatic hernias to evaluate its safety, efficacy and outcomes.
INTRODUCTION
Diaphragmatic hernia can be congenital (1 in 2500 newborns) [1] or acquired (5% of trauma) [2] that permit passage of abdominal contents into the chest cavity. Clinical presentation may range from asymptomatic cases to serious respiratory or gastrointestinal symptoms. Diagnosis is early in the case of congenital diaphragmatic hernia, whereas it is relatively delayed in the case of diaphragmatic rupture, even for years following trauma. The diagnosis of diaphragmatic hernia is based on clinical findings and is confirmed by plain X-ray film and computed tomography (CT) scan. Surgical repair of diaphragmatic hernias is indicated even in asymptomatic patients because of the danger of intestinal incarceration/strangulation or respiratory compromise [3]. Surgical repair typically involves primary or patch closure of the diaphragm through an open or endoscopic abdominal or thoracic approach or the combination. Laparoscopic diaphragmatic hernia repair is increasingly reported to be an acceptable and safe alternative to open surgical repair [4].
Here, we describe a series of four patients of diaphragmatic hernia managed by laparoscopic approach over 3-year period in our institute in an attempt to evaluate its safety, efficacy and outcomes.
CASE SERIES
A retrospective analysis was carried out to review records of patients who presented to our department over a period of 3 years from December 2017 to January 2020. All patients with diaphragmatic hernias were included in the study. Preoperative diagnosis of diaphragmatic hernia was based on history, clinical examination and radiological investigations (chest X-ray and CT) (Figs 1 and 2).
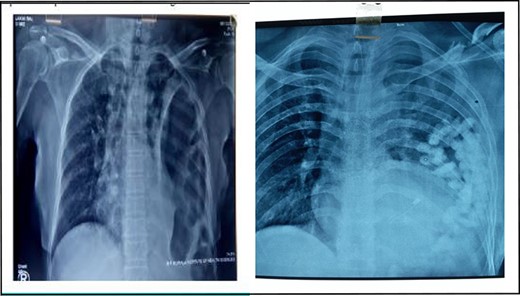
X-ray chest showing collapsed left lung with herniated bowel loops in left thoracic cavity.
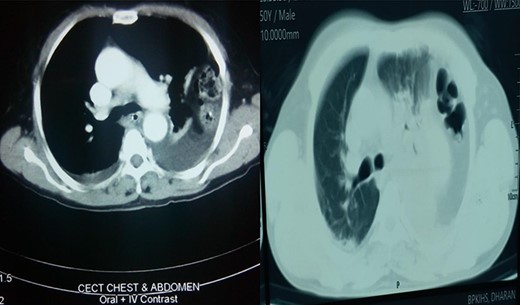
Axial section showing collapsed left lung with bowel in left thoracic cavity.
Patient demographics and hernia types were noted (Table 1). Routine blood investigations and electrocardiogram were carried out in all patients.
| Age/Gender . | Symptoms . | Type of hernia . |
|---|---|---|
| 67 years/Female | Discomfort over left chest | Left-sided traumatic diaphragmatic hernia |
| 58 years/Male | Ill-defined lump in left lumber region mimicking as a lumbar hernia | Left-sided spontaneous diaphragmatic hernia |
| 50 years/Male | Dyspnoea | Left-sided traumatic diaphragmatic hernia |
| 45 years/Male | Dyspnoea | Left-sided traumatic diaphragmatic hernia |
| Age/Gender . | Symptoms . | Type of hernia . |
|---|---|---|
| 67 years/Female | Discomfort over left chest | Left-sided traumatic diaphragmatic hernia |
| 58 years/Male | Ill-defined lump in left lumber region mimicking as a lumbar hernia | Left-sided spontaneous diaphragmatic hernia |
| 50 years/Male | Dyspnoea | Left-sided traumatic diaphragmatic hernia |
| 45 years/Male | Dyspnoea | Left-sided traumatic diaphragmatic hernia |
| Age/Gender . | Symptoms . | Type of hernia . |
|---|---|---|
| 67 years/Female | Discomfort over left chest | Left-sided traumatic diaphragmatic hernia |
| 58 years/Male | Ill-defined lump in left lumber region mimicking as a lumbar hernia | Left-sided spontaneous diaphragmatic hernia |
| 50 years/Male | Dyspnoea | Left-sided traumatic diaphragmatic hernia |
| 45 years/Male | Dyspnoea | Left-sided traumatic diaphragmatic hernia |
| Age/Gender . | Symptoms . | Type of hernia . |
|---|---|---|
| 67 years/Female | Discomfort over left chest | Left-sided traumatic diaphragmatic hernia |
| 58 years/Male | Ill-defined lump in left lumber region mimicking as a lumbar hernia | Left-sided spontaneous diaphragmatic hernia |
| 50 years/Male | Dyspnoea | Left-sided traumatic diaphragmatic hernia |
| 45 years/Male | Dyspnoea | Left-sided traumatic diaphragmatic hernia |
Initially, laparoscopic approach was opted for all four cases. In three cases, just laparoscopic approach was successful completely, whereas one case required addition of a minithoracotomy on laparoscopic approach (a hybrid technique) to reduce the content. The defects were repaired with polypropylene suture and strengthened with mesh. Details of operative procedures, postoperative complication (if any), pain score (visual analogue scale [VAS]-score) on first postoperative day, length of hospital stay and operative time were noted (Table 2).
| S.N. . | Contents . | Defect size (cm) . | Type of mesh . | Size of mesh (cm) . | Postoperative complication . | Pain on first postoperative day (VAS score) . | Postoperative hospital stay (day) . | Operative time (minute) . |
|---|---|---|---|---|---|---|---|---|
| 1 | Stomach, splenic flexure of colon, omentum, spleen | 6 × 4 | Composite mesh | 15 × 15 | None | 3 | 4 | 180 |
| 2 | Omentum | 4 × 3 | Polypropylene mesh | 10 × 15 | None | 2 | 3 | 120 |
| 3 | Omentum, transverse colon, small bowel | 3 × 3 | Composite mesh | 10 × 15 | None | 3 | 3 | 90 |
| 4 | Stomach, omentum, transverse colon | 5 × 4 | Composite mesh | 10 × 15 | None | 2 | 3 | 120 |
| S.N. . | Contents . | Defect size (cm) . | Type of mesh . | Size of mesh (cm) . | Postoperative complication . | Pain on first postoperative day (VAS score) . | Postoperative hospital stay (day) . | Operative time (minute) . |
|---|---|---|---|---|---|---|---|---|
| 1 | Stomach, splenic flexure of colon, omentum, spleen | 6 × 4 | Composite mesh | 15 × 15 | None | 3 | 4 | 180 |
| 2 | Omentum | 4 × 3 | Polypropylene mesh | 10 × 15 | None | 2 | 3 | 120 |
| 3 | Omentum, transverse colon, small bowel | 3 × 3 | Composite mesh | 10 × 15 | None | 3 | 3 | 90 |
| 4 | Stomach, omentum, transverse colon | 5 × 4 | Composite mesh | 10 × 15 | None | 2 | 3 | 120 |
| S.N. . | Contents . | Defect size (cm) . | Type of mesh . | Size of mesh (cm) . | Postoperative complication . | Pain on first postoperative day (VAS score) . | Postoperative hospital stay (day) . | Operative time (minute) . |
|---|---|---|---|---|---|---|---|---|
| 1 | Stomach, splenic flexure of colon, omentum, spleen | 6 × 4 | Composite mesh | 15 × 15 | None | 3 | 4 | 180 |
| 2 | Omentum | 4 × 3 | Polypropylene mesh | 10 × 15 | None | 2 | 3 | 120 |
| 3 | Omentum, transverse colon, small bowel | 3 × 3 | Composite mesh | 10 × 15 | None | 3 | 3 | 90 |
| 4 | Stomach, omentum, transverse colon | 5 × 4 | Composite mesh | 10 × 15 | None | 2 | 3 | 120 |
| S.N. . | Contents . | Defect size (cm) . | Type of mesh . | Size of mesh (cm) . | Postoperative complication . | Pain on first postoperative day (VAS score) . | Postoperative hospital stay (day) . | Operative time (minute) . |
|---|---|---|---|---|---|---|---|---|
| 1 | Stomach, splenic flexure of colon, omentum, spleen | 6 × 4 | Composite mesh | 15 × 15 | None | 3 | 4 | 180 |
| 2 | Omentum | 4 × 3 | Polypropylene mesh | 10 × 15 | None | 2 | 3 | 120 |
| 3 | Omentum, transverse colon, small bowel | 3 × 3 | Composite mesh | 10 × 15 | None | 3 | 3 | 90 |
| 4 | Stomach, omentum, transverse colon | 5 × 4 | Composite mesh | 10 × 15 | None | 2 | 3 | 120 |
Surgical technique
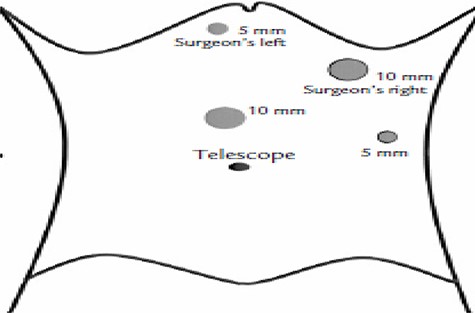
After obtaining informed consent, procedures were performed under general anaesthesia with endotracheal intubation. Four ports were placed as shown in Fig. 3.
Patients were placed in right lateral position with head end slightly elevated (20–30°). The defects were identified, contents (if any) were reduced and the defects were closed with polypropylene suture (Fig. 4).
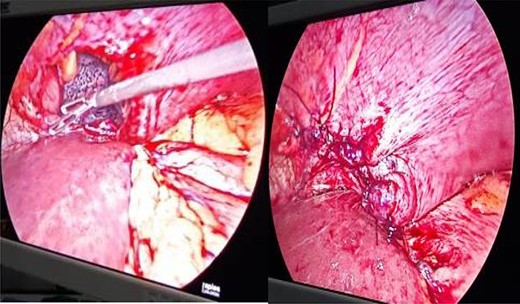
Defect in left hemidiaphragm with visible collapsed lung and closure of defect.
Closed defects were strengthened with mesh (Fig. 5).
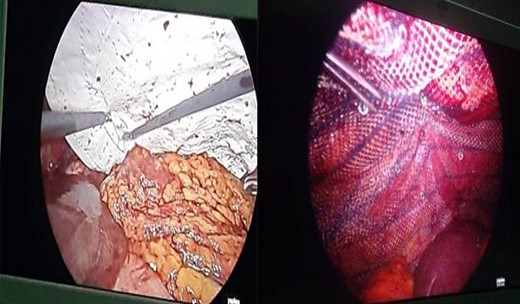
Strengthening of defect closure site with composite and polypropylene mesh.
All patients received injectable analgesics for the first 24 h after surgery and then received oral analgesics as per need. Postoperative pain was evaluated using a VAS. The operative time was defined as the time from initial skin incision to completion of skin closure. The length of stay was defined as the number of days in hospital after the operative procedure.
RESULTS
The mean age of patients was 55 years (range, 45–67 years). Half of patients had complain of chest discomfort, whereas remaining half had dyspnoea, aggravated following meal. The mean defect size was 4 cm (range, 3–6 cm), and the mean operating time was 125.7 min (range, 90–180 min). Composite mesh was used in all cases except for one, where polypropylene mesh was used due to cost factor. The mean hospital stay and pain score on first postoperative day were 3.25 days (range, 3–4 days) and 2.5 (range, 2–3). One patient required chest tube placement. There were no major postoperative complications.
DISCUSSION
Diaphragmatic hernia can be either congenital or acquired. Acquired hernia can be primary/spontaneous or secondary. Congenital diaphragmatic hernia in adulthood can occur through an anterior parasternal Morgagni foramen or through a posterolateral, mainly left sided, named as Bochdalek hernia [5]. Blunt trauma of the lower chest and upper abdomen is the major cause of diaphragmatic rupture and hernia. Traumatic diaphragmatic hernias are produced by a sudden increase in the pleuroperitoneal pressure gradient at areas of potential weakness along embryological points of fusion. A spontaneous rupture implies the absence of trauma, but there is always possibility of forgotten trauma in past or structural origin [6].
Diagnosis is based on the clinical presentation and confirmed by imaging such as chest X-ray (nasogastric tube insertion), abdominal CT scan and abdominal magnetic resonance imaging. Common radiological findings include elevated hemidiaphragm, blunting of the costophrenic angle, distortion of the diaphragm borders, curling of gastric tube into the thorax, mediastinal shift, pleural effusion or presence of air-filled gastrointestinal structures in the thoracic cavity.
The most accurate method of making the diagnosis of diaphragmatic hernia is exploration in operation theatre. The management of diaphragmatic hernia is surgical and typically involves primary or patch closure of the diaphragm through an open or endoscopic (abdominal or thoracic approach) or combined techniques.
Although there are few studies in literature describing laparoscopic approach in diaphragmatic hernia repair, we presented our experience and found it to have all the advantages of minimal access surgery and to be a safe procedure.
ETHICAL APPROVAL
Patient’s information has been de-identified to the best of our ability to protect his privacy.
CONFLICT OF INTEREST STATEMENT
None declared.



