-
PDF
- Split View
-
Views
-
Cite
Cite
Yasmine Laraqui Housseini, Hafsa Elouazzani, Laila Laraqui Housseini, Meriem Cherkaoui, Fouad Zouaidia, Pelvic angiomyofibroblastoma: an unusual case report, Journal of Surgical Case Reports, Volume 2020, Issue 5, May 2020, rjaa051, https://doi.org/10.1093/jscr/rjaa051
Close - Share Icon Share
Abstract
Angiomyofibroblastoma is a rare mesenchymal benign tumor that frequently occurs in young- to middle-aged women, arising from the genital tract. There are many overlapping radiological and immunohistochemical features with other stromal cell lesions, making the diagnosis difficult. We report here a case of a 29-year-old woman admitted for a pelvic mass, in whom, the histopathological and immunohistochemical studies led to the diagnosis of angiomyofibroblastoma.
INTRODUCTION
Angiomyofibroblastoma is an unusual and rare benign mesenchymal benign tumor arising predominantly in the vulvo-vaginal region, perineum and uterin cervix, but it rarely occurs in the pelvis or retroperitoneum. It belongs to the genital mesenchymal tumors group, especially cellular angiofibromas and aggressive angiomyxomas from which it must be differentiated.
CASE REPORT
A 29-year-old woman with 6 months’ history of a pelvic heaviness sensation. She had no familiar or personal medical history and her menstrual cycle was regular. Physical examination was normal.
Ultrasonography showed an oval, lobulated mixed echogenicity pelvic mass and well demarcated. The tumor was moderately enhanced on contrast enhanced computed tomography (CT).
The patient underwent a laparotomy which showed a regular-shaped tumor pseudo-encapsulated with no invasion to the peripheral tissues. Complete local resection was made.
Approximately, the tumor measured 15-cm-long axis and was well demarcated without veritable capsule. The cut surface appeared yellowish white and homogeneous with no hemorrhage or necrosis (Fig. 1).

Approximately, the mass measured 15-cm-long axis showing well demarcated tumor without veritable capsule. The cut surface appears yellowish white and homogeneous with no hemorrhage or necrosis.
Histopathological examination appeared well demarcated and showed alternation of hyper- and hypocellular areas, with abundant blood vessels (Fig. 2a). The stroma appeared edematous. Tumor cells were spindle shaped with fine chromatin (Fig. 2b). There were no mitotic figures observed.
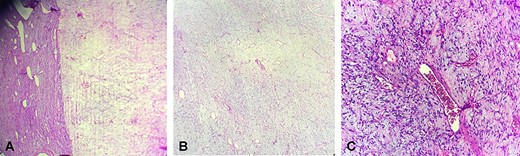
Microscopically, (a) showed alternation of hyper- and hypocellular areas (hematoxylin and eosin stain X10), (b) with spindle-shaped tumor cells and abundant blood vessels (hematoxylin and eosin stain X20)
Immunohistochemical study revealed that the tumor cells were positive for estrogen and progesterone receptors, CD34 (Fig. 3a) and desmin (Fig. 3b). There were negative for smooth muscle actin and PS-100.
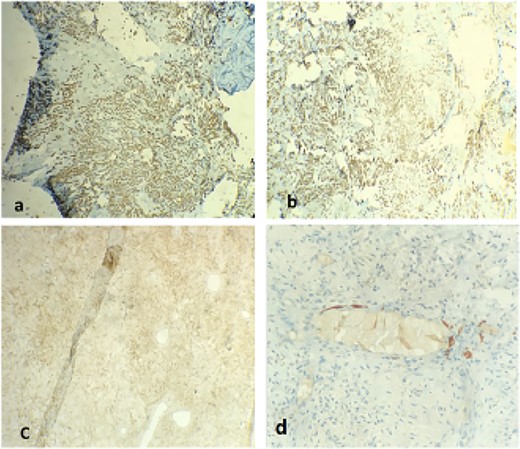
Positive staining with CD34 (a), desmin (b), progesterone receptor (c), estrogen receptor (d)
Well-demarcated lesion, histopathological findings with no mitosis and immunohistochemical results permit to make the final diagnosis.
Postsurgery evolution was favorable.
DISCUSSION
Angiomyofibroblastoma is an idiopathic unusual benign soft tissue tumor. Due to its rarity, no statistical data are available about its incidence. It occurs in young- to middle-aged women, during the reproductive period, between 20 and 50 years, and rarely in male patients [1].
Clinically, the tumor is revealed by a pelvic sensation of painless heaviness or may be asymptomatic [2]. Sometimes, it may present with obstructive symptoms like dysuria when it is located in the cervix, uterin or urethral region.
It is frequently located in the superficial regions of the lower female genital tract and is therefore easily detected. However, some tumors may be detected after reaching a massive size when it is located in the pelvis, peritoneal cavity or ilia fossa. Until there, only four cases of pelvic angiomyofibroblastoma have been reported [3].
On ultrasound, angiomyofibroblastomas appear as a mixed echogenicity soft tissue mass which is correlated with pathological examination showing inhomogeneous hyper and hypocellular areas. On CT, angiomyofibroblastoma most likely present as hypo attenuating mass with moderate to strong enhancement, reflecting the prominent vascularity of this tumor. Magnetic resonance imaging shows isointense to skeletal muscles on T1 and hypointense on T2-weighted images. Postcontrast images may show strong enhancement [4].
Therefore, the radiological characteristics of angiomyofibroblastomas may help on the diagnosis but are not specific to angiomyofibroblastoma, and it is important to distinguish this entity from other mesenchymal tumors because of the differences in therapeutic management.
Approximately, these tumors measure generally <5 cm but dimensions may be ranged from 3.8 to 25 cm. They are typically well demarcated with rubbery consistence and pink color.
On the histopathological study, angiomyofibroblastoma appears well defined and characterized by alternating hyper- and hypocellular edematous areas with abundant thin-walled blood vessels. The tumor cells are spindle-shaped and with fine chromatin and inconspicuous nucleoli. Mitotic figures are rare or absent [1].
Immunohistochemical profile of angiomyofibroblastoma is characterized by positive staining for estrogen and progesterone receptors: vimentine and desmin [5].
It is paramount to differentiate angiomyofibroblastoma from other more aggressive mesenchymal tumors such as cellular angiofibromas and angiomyxomas.
Presence of spindle cell lipomas in cellular angiofibroma and its negative staining for estrogen and progesterone receptors permit to distinguish it from angiomyofibroblastoma [1].
Differentiation between angiomyofibroblastoma and deep angiomyxoma could be more difficult because of their common characteristics as the age at presentation, location, clinical presentation and pathological findings. However, deep angiomyxoma is a malignant neoplasm with a high risk of recurrence. Histopathological study permits to distinguish between these two entities. Tumor cells in deep angiomyxoma are sparsely and diffusely distributed without the characteristic of alternating cellular areas and cells aggregation around vessels encountered in angiomyofibroblastoma. Angiomyofibroblastomas show less distinctive myxoïd degeneration than deep angiomyxomas. Immunohistochemical study is not contributory on the differential diagnostic. In fact, desmin expression was positive for some cases of deep angiomyxomas and often positive for hormonal receptors. Thus, differentiating between angiomyofibroblastoma and deep angiomyxoma is mostly based on the appearance of the tumor margins that are well demarcated in angiomyofibroblastomas [4].
The diagnosis of dedifferentiated liposarcoma should also be mentioned because of its usually retro-peritoneal location. It is a liposarcoma with a well-differentiated component juxtaposed with high grade nonlipogenic sarcoma areas. They can currently be diagnosed on the basis of MDM2 amplification even in the case of nonlipogenic undifferentiated sarcoma without any atypical adipocytic component [6].
Gastrointestinal stromal tumors (GISTs) may rarely present as a pelvic mass, leading to challenging diagnostic. Seventy percent of GISTs show spindle cell proliferation and must be taken into account in the differential diagnosis. However, CD117 is a specific marker for this tumor, positive in 95% of GISTs, allowing to make the diagnosis [7].
In perineum regions, a benign neoplasm of dendritic fibromyxolipoma should be differentiated from angiomyofibroblastoma. Histopathological and immunohistochemical findings permit easily the distinction between angiomyofibroblastoma and dendritic fibromyxolipoma. In fact, dendritic fibromyxolipoma tumor cells are small spindle or stellate cells variably associated with mature adipose tissue evolving within an abundant collagenized and myxoïd stroma. Immunohistochemical study shows a positive staining for CD34, vimentine and Bcl2 antibodies, and negative for desmin and smooth muscle actin [8].
Angiomyofibroblastoma therapeutic management consists on a curative complete surgical resection with no risk of recurrence or metastasis after the surgery [5].
CONCLUSION
Angiomyofibroblastoma is a tumor occurring with predilection in the perineal and pelvic region of women. It is rare but benign tumor that needs to be differentiated from other soft tissues tumors that may be more aggressive because of the differences in surgical treatment and clinical course.
CONFLICT OF INTEREST STATEMENT
This case report was approved by the Ethics Committee of Faculty of Medicine and Pharmacy Mohammed V University Rabat. Additional patient consent for this retrospective study was not required.
FUNDING
None.



