-
PDF
- Split View
-
Views
-
Cite
Cite
Aikaterini K Kolia, Vasileios Kalles, Constantinos G Zografos, Alexandros Chamzin, Nikolaos V Michalopoulos, Giant phyllodes tumor occupying the whole breast in a young female: feasibility of mastectomy and immediate reconstruction, Journal of Surgical Case Reports, Volume 2020, Issue 4, April 2020, rjz410, https://doi.org/10.1093/jscr/rjz410
Close - Share Icon Share
Abstract
Giant phyllodes tumors are rare fibroepithelial breast neoplasms typically >10 cm by definition. The best investigation for preoperative diagnosis is core biopsy, although it is often difficult for the pathologist to distinguish fibroadenomas from phyllodes tumors and determine the level of malignant potential. The wide excision is the appropriate therapy for phyllodes tumors taking into consideration that mastectomy may be required for huge phyllodes tumors. In the modern era of breast tissue expanders and breast implants, immediate breast reconstruction is feasible. We present a case report of a patient with a giant phyllodes tumor of 24 cm diameter who underwent mastectomy and immediate breast reconstruction with breast tissue expander.
INTRODUCTION
Fibroepithelial lesions are biphasic tumors consist of both epithelial and stromal component. The main occupants of this heterogeneous type of tumors are fibroadenomas and rarer phyllodes tumors. Stromal cellularity and atypia are evaluated in fibroepithelial lesions. It may be difficult for the pathologists to distinguish cellular fibroadenomas from low-grade phyllodes tumors on core needle biopsies due to the overlapping features of these entities. However, studies have shown that greater agreement exists when it comes for distinguishing the above entities from borderline or malignant phyllodes tumors.
Phylloides tumors are rare account for <1% of breast tumors. They were first described by Johannes Muller in 1838 named as cystosarcoma phyllodes. The World Health Organization (WHO) classification of tumors has recommended criteria for diagnosis and grading of phyllodes tumors. They are subclassified as low-grade (benign), high-grade (malignant) and intermediate-grade (borderline) according to pushing or infiltrative margins, nuclear atypia and number of mitoses per 10 high-powered fields (hpf). Recurrence rates in the literature are 10–17, 14–25 and 23–30% for benign, borderline and malignant phyllodes tumors, respectively, while distant metastases are presented in 9% of malignant tumors mainly in lungs and bones. The recurrent tumors may be of a higher grade than the primary tumor’s grade.
CASE REPORT
A 38-year-old female was referred to the Outpatient Breast Clinic due to having a huge mass on the right breast for >2 years. On examination, a firm lobulated huge mass was observed with superficial veins on the breast being significantly bulging and a skin ulcer in the lower outer quadrant (Fig. 1). Neither clinically positive lymph nodes nor nipple discharge were found on clinical examination.
The most recent chest computed tomography indicated a swollen anterior chest wall with areas of low density, interpreted by radiologist as possible invasion of pectoralis major muscle. Preoperative examination tests did not prove any distant metastases. The patient underwent fine needle aspiration that revealed stromal cells, often accompanied by large, folded sheets of epithelium suggesting fibroepithelial lesion.

A 38-year-old female with phyllodes tumor occupying the right breast.
Two years ago, the patient had undergone a mammogram (Fig. 2), which had shown breast asymmetry due to a large lobulated mass with smooth and circumscribed margins.
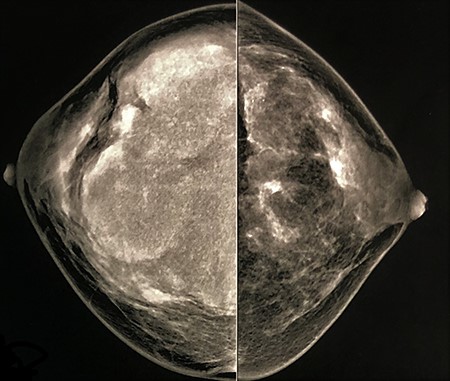
Mammogram (CC view) performed 2 years ago had shown lobulated mass with smooth and circumscribed margins.
Surgery was scheduled after discussion with the patient who was explained that breast reconstruction might not be feasible due to the possible involvement of pectoralis major muscle. Informed consent was obtained from the patient. Wide mastectomy was performed. At this point, it has to be underlined that dissection was performed carefully since there were multiple bulging vessels. Trying to conserve pectoralis major muscle for reconstruction only a superficial layer of muscle fibers was resected.
Macroscopically, surgical margins were free. Reconstruction with tissue expander was decided and it was inserted beneath pectoralis major. Skin flaps were closed under some degree of tension after the placement of surgical drains. Postoperatively, the patient recovered with no complications (Fig. 3).

Two days after mastectomy and breast reconstruction with tissue expander.
Histology revealed phyllodes tumor of 26 cm in maximum diameter with moderate cellularity and atypia, without invasive growth pattern. Heterogeneity was observed with regard to mitotic activity but not <5–7 mitoses/10 hpf were found so that the tumor was categorized as borderline phyllodes tumor according to WHO.
DISCUSSION
Surgical management of phyllodes tumors requires wide excision with tumor free margins of 10 mm conserving the breast tissue for oncoplastic surgery or mastectomy either it comes to giant phyllodes or cosmetic results cannot be achieved [1–3], although there are recent studies that provide the data for no local control advantage of 1 cm free margin over a thinner one [4].
In cases of primary tumors or local recurrences where mastectomy is required, immediate reconstruction may be the preferred option. Axillary staging is not recommended for phyllodes tumors.
The precise role of adjuvant radiotherapy is controversial. Although radiotherapy has not been approved having impact on disease-free or overall survival, data provided from studies supports that radiotherapy reduces local recurrences particularly for patients with close surgical margins or positive margins for borderline and malignant tumors particularly after breast conserving surgery [5, 6]. However, no randomized data exist about radiotherapy benefits. Current guidelines suggest radiotherapy only when local control is desired and surgical treatment is not possible [7–9].
Finally, little evidence exists about postoperative chemotherapy for phyllodes tumors. Currently, its use with doxorubicin and ifosfamide is limited to therapy of distant metastases. Hormonal therapy has no role on phyllodes tumors [10].
In our case, a 38-year-old woman with borderline phyllodes tumor underwent mastectomy due to the giant size of the tumor (26 cmx). Although axillary sampling is not an option in clinically absent invasion of lymph nodes (most of distant metastases in phyllodes tumors are hematogeneous), two lymph nodes, negative for invasive component, were excised en block with mastectomy specimen. Preoperative imaging findings indicated possible invasion of pectoralis major. However, intraoperative findings of no extended invasion of the muscle did not consist problem for performing immediate breast reconstruction with tissue expander. Histology report revealed free surgical margins. Due to existing data, the patient did not undergo radiotherapy.
ACKNOWLEDGEMENT
We are grateful to the patient for allowing this report.
Conflict of interest statement
None declared.



