-
PDF
- Split View
-
Views
-
Cite
Cite
Tadashi Igarashi, Takao Kaneko, Shu Yoshizawa, Kazutaka Takada, Yu-uki Matsu-ura, Hiroyasu Ikegami, Yoshiro Musha, Autologous chondrocyte implantation with a Reveille cartilage processor for articular cartilage injury: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 4, April 2020, rjaa074, https://doi.org/10.1093/jscr/rjaa074
Close - Share Icon Share
Abstract
Autologous chondrocyte implantation (ACI) is an important operative option when repairing cartilage defects of the knee. This report introduces a new product development with one-stage ACI using a Reveille Cartilage Processor (Reveille CP) as well as the assessment of MRI and clinical results at a 1-year follow-up. The report compared cases between a 42-year-old female who underwent ACI surgery using Reveille CP and a 51-year old female who received treatment with two-stage ACI of tissue-engineered cartilage-like tissue (J-TEC Autologous Chondrocyte Cultured Cartilage [JACC]). One year after JACC, magnetic resonance imaging (MRI) showed signal intensity area in the grafted area, while patients with Reveille CP showed greater thickness than the surrounding healthy cartilage. The Lysholm, pain and QOL scores of Knee Injury and Osteoarthritis Outcome (KOOS) at one 1 year after surgery with Reveille CP were higher than JACC.
INTRODUCTION
Articular cartilage lacks blood vessels, nerves and lymphatic vessels and has a very poor ability to self-repair [1, 2]; therefore, articular cartilage injury is a devastating problem for patients.
Surgical treatment options for articular cartilage injury include bone marrow stimulation technique (e.g. microfracture) [3, 4], direct chondral replacement (e.g. allograft transplantation and mosaicplasty) [5] and autologous chondrocyte implantation (ACI) using cultured cells. Microfracture and mosaicplasty techniques contain treatment obstacle, including the regeneration of fibrocartilage in microfracture technique and the limitation to treat larger chondral lesions [6]. ACI, first reported by Brittberg et al. [7], has been performed for more than 20 000 patients worldwide for 20 years, although it has yet to be applied for knee osteoarthritis [8, 9]. The outcomes of ACI are not necessarily positive [10, 11].
| . | Reveille pre-op . | JACC pre-op . |
|---|---|---|
| Tegner score (point) | 5.0 | 7.0 |
| Range of motion (degree) | 0–145 | 0–140 |
| MOCART score (point) | 10.0 | 5.0 |
| Lysholm score (point) | 50.0 | 45.0 |
| KOOS score (%) | ||
| Pain | 35.7 | 35.7 |
| Symptoms | 16.7 | 27.8 |
| ADL | 26.5 | 41.2 |
| Sport/recreation | 5.0 | 15.0 |
| QOL | 6.3 | 12.5 |
| . | Reveille pre-op . | JACC pre-op . |
|---|---|---|
| Tegner score (point) | 5.0 | 7.0 |
| Range of motion (degree) | 0–145 | 0–140 |
| MOCART score (point) | 10.0 | 5.0 |
| Lysholm score (point) | 50.0 | 45.0 |
| KOOS score (%) | ||
| Pain | 35.7 | 35.7 |
| Symptoms | 16.7 | 27.8 |
| ADL | 26.5 | 41.2 |
| Sport/recreation | 5.0 | 15.0 |
| QOL | 6.3 | 12.5 |
| . | Reveille pre-op . | JACC pre-op . |
|---|---|---|
| Tegner score (point) | 5.0 | 7.0 |
| Range of motion (degree) | 0–145 | 0–140 |
| MOCART score (point) | 10.0 | 5.0 |
| Lysholm score (point) | 50.0 | 45.0 |
| KOOS score (%) | ||
| Pain | 35.7 | 35.7 |
| Symptoms | 16.7 | 27.8 |
| ADL | 26.5 | 41.2 |
| Sport/recreation | 5.0 | 15.0 |
| QOL | 6.3 | 12.5 |
| . | Reveille pre-op . | JACC pre-op . |
|---|---|---|
| Tegner score (point) | 5.0 | 7.0 |
| Range of motion (degree) | 0–145 | 0–140 |
| MOCART score (point) | 10.0 | 5.0 |
| Lysholm score (point) | 50.0 | 45.0 |
| KOOS score (%) | ||
| Pain | 35.7 | 35.7 |
| Symptoms | 16.7 | 27.8 |
| ADL | 26.5 | 41.2 |
| Sport/recreation | 5.0 | 15.0 |
| QOL | 6.3 | 12.5 |
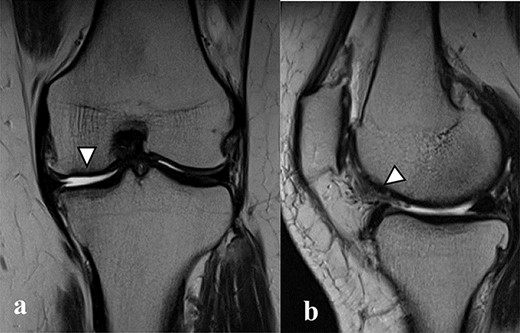
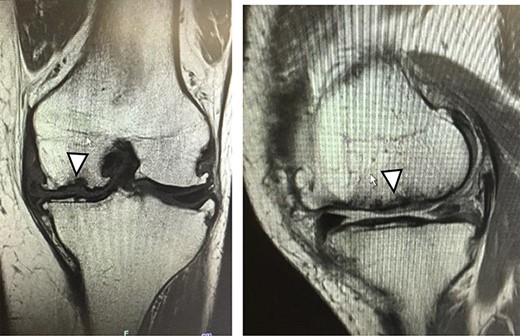
There were cartilage defects (arrowhead) in the medial femoral condyle and trochlea of the left knee (a, b).
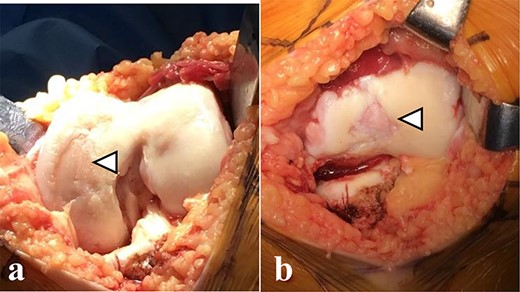
Articular cartilage injury was shown in the medial femoral condyle (arrowhead) (2.5 × 3.5 cm; Outerbridge classification, Grade III) and trochlea (arrowhead) (1.3 × 1.7 cm; Outerbridge classification, Grade III) (a, b).
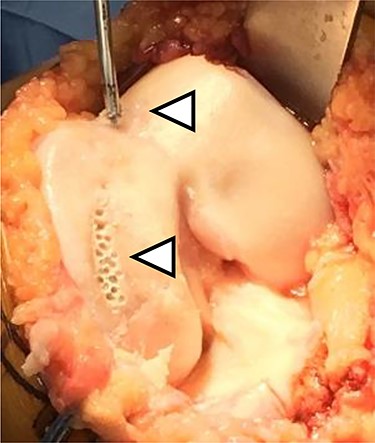
The microfracture was performed using a 4-mm power pick at the cartilage defect (arrowhead).
Recently, there are many reports on alternatives to the current methods of ACI. Ito et al. [12] reported that the manufactured layered chondrocyte sheets can contribute to tissue repair at the sites of articular cartilage injury. Sekiya et al. [13] demonstrated that patients with cartilage defects of the knee benefit from arthroscopic transplantation of autologous synovial mesenchymal stem cells in terms of magnetic resonance imaging (MRI) and clinical findings. Takazawa et al. [14] revealed that the two-stage implantation of tissue-engineered cartilage-like tissue (J-TEC Autologous Chondrocyte Cultured Cartilage, JACC®; Japan Tissue Engineering Co., Ltd, Aichi, Japan) for the cartilage defects of the knee was effective in short- to midterm postoperatively. This study examined a new product. Our case demonstrated a new product with one-stage ACI called Reveille Cartilage Processor (Reveille CP, Exactech, Inc., Gainesville, FL, USA) and reported the comparison between Reveille CP and JACC using MRI and clinical results at 1 year after ACI.
CASE REPORTS
Case 1
A 42-year-old female (BMI, 27.4 kg/m2) presented with 2 years of left knee medial joint pain. Active range of motion (ROM) in the left knee was from 0 to 140 degrees with no extension lag. Preoperative Tegner scores, Lysholm scores and Knee Injury and Osteoarthritis Outcome (KOOS) scores are shown in Table 1. Preoperative radiographs of the left knee joint showed mild medial osteoarthritis (OA) of the knee and hip–knee–ankle (HKA) angle of 1.5-degree varus. 1.5-Tesla MRI was performed on unit (Toshiba, Kawasaki, Japan) was used with an extremity surface coil. Proton density images were obtained using the fast spin-echo technique. A modified magnetic resonance observation of cartilage repair tissue (MOCART) system was used for the quantitative evaluation of MRI findings of the cartilage injury [15–17]. MRI showed cartilage injury of the medial femoral condyle (MFC) and trochlea of the left knee (Fig. 1).
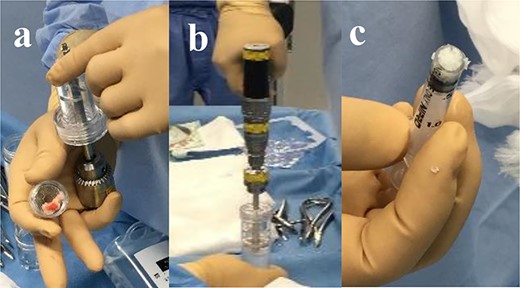
(a) Harvested cartilage fragments were loaded directly onto the Reveille CP. (b) The tissue was morselized in a sterile saline with the drill speed at 1500 rpm for 2 minutes. (c) The collected (?) volume was measured using a syringe marked at every 0.1-ml increment.
One-stage ACI using Reveille CP was performed under general anesthesia. The medial subvastus approach was used. Articular cartilage injury was shown in the trochlea (1.3 × 1.7 cm; Outerbridge classification, Grade III) and MFC (2.5 × 3.5 cm; Outerbridge classification: Grade III) (Fig. 2). We harvested the healthy cartilage (0.5 × 1.5 cm) in non-weight-bearing area of the lateral femoral condyle, and the microfracture was performed at a 4-mm power pick at the cartilage lesion (Fig. 3). Harvested cartilage fragments were loaded directly onto the Reveille CP (Fig. 4). The tissue was morselized in a sterile saline with the drill speed at 1500 rpm for 2 minutes (Fig. 4), and the chamber was plunged through a filtration apparatus to ensure that only the decanted, particulated cartilage remained (Fig. 4). The particulates were collected into the delivery device. The collected volume was measured using a syringe marked at every 0.1-ml increment (Fig. 4). The grafted cartilage particulates at the lesion were compressed, and the bone glue was applied over the particulated tissue (Fig. 5), followed by turning off of a tourniquet. The area of grafted cartilage was confirmed so that it did not fall off. Knee joints were immobilized for 4 weeks with a soft knee brace. A ROM exercise is started with a continuous passive motion device at 3 weeks after the surgery. Partial weight-bearing (30% body weight) was allowed at 4 weeks, and full weight-bearing permission was given from 8 weeks after the surgery.
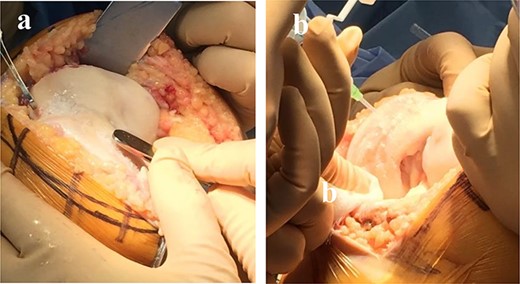
The grafted cartilage particulates at the lesion were compressed, and the bone glue was applied over the particulated tissue (a, b).
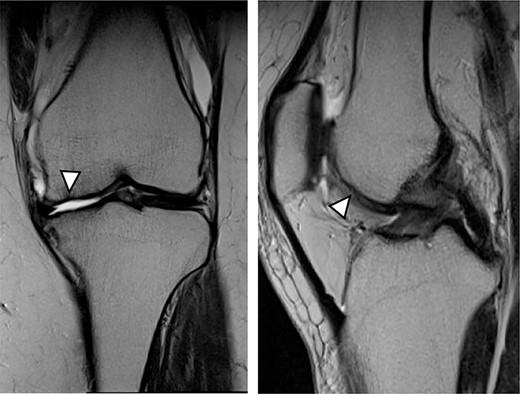
MRI showed cartilage injury of the medial femoral condyle (arrowhead).
Case 2
As a control case, a 51-year-old female (BMI, 24.1 kg/m2) presented with 4.5 years of left knee medial joint pain. Preoperative Tegner scores, Lysholm scores and KOOS scores are shown in Table 1. Preoperative radiographs of the left knee joint showed mild medial osteoarthritis (OA) of the knee and hip–knee–ankle (HKA) angle of 1.3-degree varus. MRI showed cartilage injury at the MFC (Fig. 6). Approximately 0.5 g of the healthy cartilage was harvested from less weight-bearing regions of the intercondylar notch using arthroscopy. The specimen was sent to J-TEC for cartilage culture. At 4 weeks after the harvest, the microfracture was performed at a 4-mm power pick at the cartilage lesion, and the two-stage implantation of tissue-engineered cartilage-like tissue (JACC) was performed on the cartilage injury site (4.5 × 5.5 cm; Outerbridge classification, Grade III), and then the tissue implantation site was covered with periosteum taken from the tibia of the same patient (Fig. 7). Knee joints were immobilized for 4 weeks with a soft knee brace. A ROM exercise is started with a continuous passive motion device at 3 weeks after surgery. Partial weight-bearing (30% body weight) was allowed at 4 weeks, and full weight-bearing permission was given from 8 weeks after the surgery.
Postoperative ROM, Lysholm scores and KOOS scores between cases 1 and 2 are shown in Table 2. The ROM at 1 year after Reveille CP surgery was less than that of JACC. The Lysholm, pain and QOL scores of KOOS at 1 year after Reveille CP surgery were higher than these scores of JACC (Table 2).
MRI findings at 1 year after the surgery indicated signal intensity area in the grafted area for the patient with JACC (Fig. 8), whereas the patient who underwent Reveille CP exhibited greater thickness at the grafted area as compared to the surrounding healthy cartilage (Fig. 9). The MOCART score at 1 year after the Reveille CP surgery (60 points) was higher than that of JACC (50 points).
DISCUSSION
The one-stage ACI case showed excellent results using Reveille CP at 1 year after the surgery. In JACC, the atelocollagen gel, which contains many chondrocytes, was used as the tissue-engineered cartilage for grafting. The atelocollagen gel was placed over the cartilage defect site and then covered with periosteum taken from the tibia. On the contrary, the Reveille CP was placed over the particulated cartilage containing chondrocytes by applying compression over the grafted tissue. Therefore, we confirmed that clinical scores at postoperative 1 year after Reveille CP were better than JACC and the graft area was thicker than the surrounding healthy cartilage at 1 year after Reveille CP. However, a decrease of ROM was observed, which was affected by fibrosis of the suprapatellar pouch due to postoperative immobilization for 6 weeks. The period of postoperative immobilization in JACC was 1 week.

The two-stage implantation of tissue-engineered cartilage-like tissue (JACC) for the cartilage injury of the medial femoral condyle of the left knee was performed and then covered with periosteum taken from the tibia.
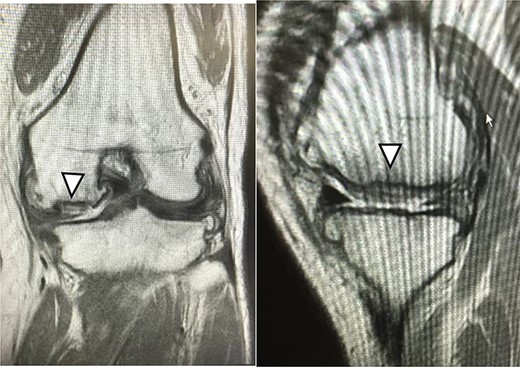
One year after JACC, MRI showed T2 high intensity area in the graft area (arrowhead).
A new product development of ACI with Reveille CP has three characteristics. The first characteristic is that Reveille CP creates autologous tissue with more surface area to absorb bioactive factors available within the marrow stimulation superclot. The second characteristic is that it creates autologous tissue grafts that retain high levels of variable, biologically competent chondrocytes. The third characteristic is that it creates autologous tissue grafts that support cellular proliferation, migration and new tissue matrix formation in culture. The adaptation in size of the cartilage defect is up to 4 cm2 for Reveille CP and 4 cm2 or higher for JACC. The advantage of Reveille CP includes one-stage surgical technique that requires no allergic test for atelocollagen gel nor periosteum sacrifice when compared with JACC. Meanwhile, Adachi et al. [17] reported that clinical data improved significantly postoperatively after implantation of tissue-engineered cartilage for full-thickness cartilage defects of the knee. In addition, good clinical outcomes were maintained for at least a median of 8.0 years, indicating the efficacy and durability of this procedure. Also, the MOCART score in case 2 improved to 75 points at 5 years after JACC surgery (Fig. 10). Knutsen et al. [18] revealed that further surgery was required in 23% of patients at 69 months after both ACI and microfracture treatments. In other words, a long-term follow-up of ACI using Reveille CP is required.
| . | Reveille 1POY . | JACC 1POY . |
|---|---|---|
| Range of motion (degree) | 0–125 | 0–140 |
| MOCART score (point) | 60.0 | 50.0 |
| Lysholm score (point) | 93.0 | 88.0 |
| KOOS score (%) | ||
| Pain | 78.6 | 67.9 |
| Symptoms | 88.9 | 88.9 |
| ADL | 91.2 | 90.3 |
| Sport/recreation | 45.5 | 46.5 |
| QOL | 75.0 | 68.8 |
| . | Reveille 1POY . | JACC 1POY . |
|---|---|---|
| Range of motion (degree) | 0–125 | 0–140 |
| MOCART score (point) | 60.0 | 50.0 |
| Lysholm score (point) | 93.0 | 88.0 |
| KOOS score (%) | ||
| Pain | 78.6 | 67.9 |
| Symptoms | 88.9 | 88.9 |
| ADL | 91.2 | 90.3 |
| Sport/recreation | 45.5 | 46.5 |
| QOL | 75.0 | 68.8 |
| . | Reveille 1POY . | JACC 1POY . |
|---|---|---|
| Range of motion (degree) | 0–125 | 0–140 |
| MOCART score (point) | 60.0 | 50.0 |
| Lysholm score (point) | 93.0 | 88.0 |
| KOOS score (%) | ||
| Pain | 78.6 | 67.9 |
| Symptoms | 88.9 | 88.9 |
| ADL | 91.2 | 90.3 |
| Sport/recreation | 45.5 | 46.5 |
| QOL | 75.0 | 68.8 |
| . | Reveille 1POY . | JACC 1POY . |
|---|---|---|
| Range of motion (degree) | 0–125 | 0–140 |
| MOCART score (point) | 60.0 | 50.0 |
| Lysholm score (point) | 93.0 | 88.0 |
| KOOS score (%) | ||
| Pain | 78.6 | 67.9 |
| Symptoms | 88.9 | 88.9 |
| ADL | 91.2 | 90.3 |
| Sport/recreation | 45.5 | 46.5 |
| QOL | 75.0 | 68.8 |
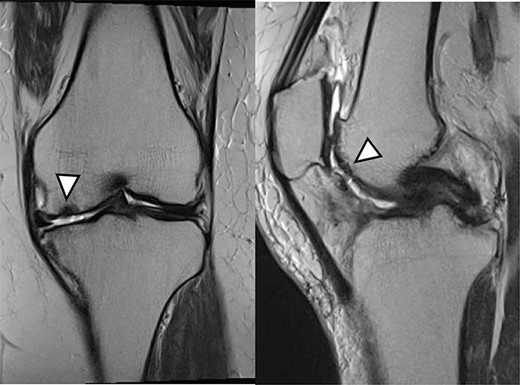
One year after Reveille CP. The graft area was thicker than surrounding healthy cartilage (arrowhead).
Five years after JACC. MRI showed the graft area was thicker than the surrounding healthy cartilage (arrowhead).
Roberts et al. [19] assessed the relative proportions of type I and II collagens and type IIA procollagen in full-depth biopsies of repair tissue in a large sample of patients treated with ACI alone (n = 55) or in combination with mosaicplasty (n = 10). Based on his study, 65% of biopsies were predominantly fibrocartilage (mostly type I collagen and IIA procollagen), 15% were hyaline cartilage (mostly type II collagen), 17% were of mixed morphology and 3% were fibrous tissue (mostly type I collagen). Most type II collagens were present 30–60 months after treatment, suggesting that cartilage repair tissue production following ACI treatment takes some years to mature.
Two weaknesses were identified in this study. First, we did not evaluate whether cartilage defects can be repaired with hyaline cartilage. Second, we did not evaluate whether glycosaminoglycan is produced from a transplanted cartilage by 3.0-Tesla MRI and Gd contrast media. Further study needs to verify these weaknesses.
These case reports assessed the result of a one-stage particulate articular cartilage implantation using Reveille CP while comparing against two-stage ACI using JACC. Early results showed marked improvement in patient-reported outcome measurements from pre-op to 1 year postoperative follow-up. MRI evaluation showed more cartilage incorporation and resolution of preoperative bony edema in Reveille CP case than the JACC case. The one-stage ACI using Reveille CP warrants further studies with a larger sample size and longer follow-up.
ACKNOWLEDGMENTS
The authors thank Hiroaki Suzuki and Jun Sekihara for their assistance in this study.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.



