-
PDF
- Split View
-
Views
-
Cite
Cite
Jonathan Keyes, Adela T Casas-Melley, Cherry Liu, Monica S Epelman, Pamela I Ellsworth, Scrotal abscess after a perforated appendicitis, Journal of Surgical Case Reports, Volume 2020, Issue 4, April 2020, rjaa058, https://doi.org/10.1093/jscr/rjaa058
Close - Share Icon Share
Abstract
Although perforated appendicitis in pediatric patients can result in a diverse array of complications, scrotal abscess is a rarely documented phenomenon. We present a case of acute scrotum after laparoscopic appendectomy. A retrospective review of prior literature on scrotal abscess secondary to perforated appendicitis was performed via PubMed to review the clinical presentation, etiology, type of treatment and outcome of pediatric patients. Patients without a patent processus vaginalis still require vigilant follow-up postoperatively to ensure timely intervention if scrotal pain develops during recovery.
INTRODUCTION
The testes develop as part of the abdominal cavity at about 9 weeks of gestation and descend into the scrotum via the processus vaginalis and thus, the processus vaginalis serves as a window of communication between the peritoneum and the scrotum until its eventual closure. A patent processus vaginalis (PPV) has been estimated to be present in 80–95% of newborn males, 60% at 1 year of age, 40% at 2 years and 15–37% persist into adulthood [1]. Abscess formation is a well-known complication of perforated appendicitis. It commonly occurs intra-abdominally. In rare cases, scrotal abscess can follow perforated appendicitis. A number of cases have been identified where a PPV was present [1–8], which allowed for the gravitational flow of intraperitoneal pus into the scrotum via the inguinal canal. We present a case of scrotal abscess following a laparoscopic appendectomy of a perforated appendix in which the PPV was not present. The case highlights the importance of ultrasound evaluation of scrotal swelling and pain in post-appendectomy in pediatric patients.
| Authors . | Age (years) . | Side affected . | Surgery (primary) . | Surgery (secondary) . | Presence of PPV . |
|---|---|---|---|---|---|
| Kynes et al. [4] | 23 months | Right | Inguinal exploration, open appendectomy | No further surgery | Yes |
| Shehzad et al. [7] | 16 | Right | Scrotal exploration, open appendectomy | No further surgery | Yes |
| Mansoor et al. [5] | 4 | Right | Scrotal exploration, open appendectomy | No further surgery | Yes |
| Saleem et al. [1] | 10 | Left | Open appendectomy | Groin exploration, scrotal incision and drainage | Yes |
| Saleem et al. [1] | 4 | Left | Open appendectomy | Groin exploration, scrotal incision and drainage | Yes |
| Bingol-Kologlu et al. [2] | 7 | Right | Appendectomy (unspecified) | Groin exploration, scrotal incision and drainage | Yes |
| Bingol-Kologlu et al. [2] | 4 | Right | Appendectomy (unspecified) | Groin exploration, scrotal incision and drainage | Yes |
| Thakur et al. [8] | 9 | Right | Open appendectomy | Inguinal incision and drainage | Yes |
| Thakur et al. [8] | 7 | Right | Laparoscopic appendectomy | Inguinal and scrotal incision and drainage | Yes |
| DeFoor et al. [3] | 11 | Left | Laparoscopic appendectomy | Scrotal incision and drainage | Yes |
| Yasumoto et al. [9] | 10 | Left | Scrotal incision and drainage | Laparoscopic appendectomy | No |
| Shahrudin et al. [6] | 3 | Right | Open appendectomy | Scrotal incision and drainage | Yes |
| McKerrow et al. [10] | 9 | Right | Open appendectomy | Scrotal incision and drainage | No |
| Authors . | Age (years) . | Side affected . | Surgery (primary) . | Surgery (secondary) . | Presence of PPV . |
|---|---|---|---|---|---|
| Kynes et al. [4] | 23 months | Right | Inguinal exploration, open appendectomy | No further surgery | Yes |
| Shehzad et al. [7] | 16 | Right | Scrotal exploration, open appendectomy | No further surgery | Yes |
| Mansoor et al. [5] | 4 | Right | Scrotal exploration, open appendectomy | No further surgery | Yes |
| Saleem et al. [1] | 10 | Left | Open appendectomy | Groin exploration, scrotal incision and drainage | Yes |
| Saleem et al. [1] | 4 | Left | Open appendectomy | Groin exploration, scrotal incision and drainage | Yes |
| Bingol-Kologlu et al. [2] | 7 | Right | Appendectomy (unspecified) | Groin exploration, scrotal incision and drainage | Yes |
| Bingol-Kologlu et al. [2] | 4 | Right | Appendectomy (unspecified) | Groin exploration, scrotal incision and drainage | Yes |
| Thakur et al. [8] | 9 | Right | Open appendectomy | Inguinal incision and drainage | Yes |
| Thakur et al. [8] | 7 | Right | Laparoscopic appendectomy | Inguinal and scrotal incision and drainage | Yes |
| DeFoor et al. [3] | 11 | Left | Laparoscopic appendectomy | Scrotal incision and drainage | Yes |
| Yasumoto et al. [9] | 10 | Left | Scrotal incision and drainage | Laparoscopic appendectomy | No |
| Shahrudin et al. [6] | 3 | Right | Open appendectomy | Scrotal incision and drainage | Yes |
| McKerrow et al. [10] | 9 | Right | Open appendectomy | Scrotal incision and drainage | No |
| Authors . | Age (years) . | Side affected . | Surgery (primary) . | Surgery (secondary) . | Presence of PPV . |
|---|---|---|---|---|---|
| Kynes et al. [4] | 23 months | Right | Inguinal exploration, open appendectomy | No further surgery | Yes |
| Shehzad et al. [7] | 16 | Right | Scrotal exploration, open appendectomy | No further surgery | Yes |
| Mansoor et al. [5] | 4 | Right | Scrotal exploration, open appendectomy | No further surgery | Yes |
| Saleem et al. [1] | 10 | Left | Open appendectomy | Groin exploration, scrotal incision and drainage | Yes |
| Saleem et al. [1] | 4 | Left | Open appendectomy | Groin exploration, scrotal incision and drainage | Yes |
| Bingol-Kologlu et al. [2] | 7 | Right | Appendectomy (unspecified) | Groin exploration, scrotal incision and drainage | Yes |
| Bingol-Kologlu et al. [2] | 4 | Right | Appendectomy (unspecified) | Groin exploration, scrotal incision and drainage | Yes |
| Thakur et al. [8] | 9 | Right | Open appendectomy | Inguinal incision and drainage | Yes |
| Thakur et al. [8] | 7 | Right | Laparoscopic appendectomy | Inguinal and scrotal incision and drainage | Yes |
| DeFoor et al. [3] | 11 | Left | Laparoscopic appendectomy | Scrotal incision and drainage | Yes |
| Yasumoto et al. [9] | 10 | Left | Scrotal incision and drainage | Laparoscopic appendectomy | No |
| Shahrudin et al. [6] | 3 | Right | Open appendectomy | Scrotal incision and drainage | Yes |
| McKerrow et al. [10] | 9 | Right | Open appendectomy | Scrotal incision and drainage | No |
| Authors . | Age (years) . | Side affected . | Surgery (primary) . | Surgery (secondary) . | Presence of PPV . |
|---|---|---|---|---|---|
| Kynes et al. [4] | 23 months | Right | Inguinal exploration, open appendectomy | No further surgery | Yes |
| Shehzad et al. [7] | 16 | Right | Scrotal exploration, open appendectomy | No further surgery | Yes |
| Mansoor et al. [5] | 4 | Right | Scrotal exploration, open appendectomy | No further surgery | Yes |
| Saleem et al. [1] | 10 | Left | Open appendectomy | Groin exploration, scrotal incision and drainage | Yes |
| Saleem et al. [1] | 4 | Left | Open appendectomy | Groin exploration, scrotal incision and drainage | Yes |
| Bingol-Kologlu et al. [2] | 7 | Right | Appendectomy (unspecified) | Groin exploration, scrotal incision and drainage | Yes |
| Bingol-Kologlu et al. [2] | 4 | Right | Appendectomy (unspecified) | Groin exploration, scrotal incision and drainage | Yes |
| Thakur et al. [8] | 9 | Right | Open appendectomy | Inguinal incision and drainage | Yes |
| Thakur et al. [8] | 7 | Right | Laparoscopic appendectomy | Inguinal and scrotal incision and drainage | Yes |
| DeFoor et al. [3] | 11 | Left | Laparoscopic appendectomy | Scrotal incision and drainage | Yes |
| Yasumoto et al. [9] | 10 | Left | Scrotal incision and drainage | Laparoscopic appendectomy | No |
| Shahrudin et al. [6] | 3 | Right | Open appendectomy | Scrotal incision and drainage | Yes |
| McKerrow et al. [10] | 9 | Right | Open appendectomy | Scrotal incision and drainage | No |
CASE PRESENTATION
An 11-year-old male presents to the Emergency Department with chief complaints of fever, abdominal pain, nausea and non-bloody vomitus. The patient has no significant past medical history except for a weight that is >95th percentile. The pain started in the periumbilical area and became more generalized. Physical exam showed right lower quadrant (RLQ) pain with guarding with positive obturator sign but no rebound tenderness. An abdominal ultrasound was performed; however, the appendix could not be visualized. The patient then underwent an abdominal computed tomography (CT) that showed a perforated appendicitis. He was immediately taken to the operating room for laparoscopic appendectomy. A perforated appendix with free intraperitoneal pus identified in multiple abdominal quadrants during the operation. The appendix was successfully removed and the patient was transferred to post anesthesia care unit (PACU) in stable condition for recovery. Overnight, the patient developed increasing left scrotal swelling with mild tenderness. Doppler ultrasound showed normal arterial and venous blood flow in both testes, but demonstrated diffuse scrotal wall thickening and inflammation, more pronounced on the left. The patient’s condition failed to improve over the course of next few days and urology was consulted. Repeat ultrasound and a CT scan was obtained, which demonstrated a left intra-scrotal abscess (Figs 1 and 2). Surgical exploration was recommended. At the time of left scrotal exploration, a large intra-scrotal abscess extending into the inguinal canal was identified. Careful examination failed to identify a PPV. The abscess fluid was cultured, drained and the wound irrigated with antibiotic solution. A Penrose drain was placed. The cultures reported rare anaerobic growth of gram-negative rods. He was placed on meropenem and vancomycin at the recommendation of infectious disease. The drain was left in place and he was discharged home with amoxicillin–clavulanate. The drain was later removed on postoperative day five and he recovered fully without sequelae.
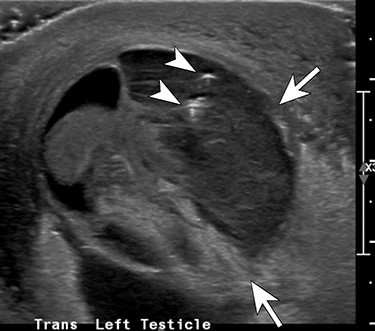
Transverse ultrasound image through the left hemiscrotum shows a complex fluid collection (arrows) including a few internal foci of gas (arrowheads) and debris.

Enhanced axial CT scan image through the scrotum re-demonstrates the complex left hemiscrotal collection (arrows) with internal locules of gas (arrowheads).
DISCUSSION
Intra-abdominal abscess is a well-known complication of perforated appendicitis; however, extra-abdominal inflammation such as scrotal abscess is less frequently documented. A literature review of pediatric reports published in English on PubMed using the search term ‘scrotal abscess appendix’ (http://www.ncbi.nlm.gov/pubmed; accessed 27 October 2019) showed 13 cases in which the patient developed scrotal abscess after an appendiceal perforation (Table 1). In three cases [4,5,7], no secondary surgery was performed because a scrotal abscess was identified at the time of the appendectomy. In one case in which the presenting symptoms raised a suspicion for testicular torsion, the initial approach was via a scrotal incision and drainage followed by appendectomy [9]. Unlike most cases reported in the literature, this case highlights that scrotal abscesses can occur post-appendectomy on the left side and in the absence of a PPV on gross examination.
Although the processus vaginalis obliterates in most individuals, 15–37% may persist into adulthood [1]. The concurrent finding of a PPV and a perforated appendix should alert physicians to the risk scrotal abscess formation. The location of the appendix allows for gravitational flow through a PPV into the right hemiscrotum. In our case, the patient did not have an identifiable PPV and the abscess was in the left hemiscrotum. Although our patient is not the first case that developed a scrotal abscess in the absence of a PPV [9,10], it is a less common occurrence compared to a PPV. During a laparoscopic procedure for perforated appendicitis, it is possible that irrigation of the abdominal cavity may have flushed the pus from the right to the left side, which then resulted in contaminated fluid in the left pelvic and inguinal region. Thus, careful inspection of the abdominal during irrigation and aspiration is important to ensure that all purulent material is evacuated. Given the patient’s obesity, another plausible explanation is that the higher insufflation pressure needed during laparoscopy resulted in a translocation of intra-abdominal bacteria through the closed processus vaginalis. Lastly, although no detectable patency was identified in the processus vaginalis on gross inspection at the time of surgery, a micro-perforation in the PPV may have been present allowing for purulent material to pass into left inguinal region and scrotum. Our case, as well as those presented by Yasumoto et al. and McKerrow et al., demonstrated that the absence of a defined PPV does not prevent postoperative scrotal abscess formation [9,10]. Additionally, three abscesses were on the left side with a PPV have been described, and one case on the left side without observable PPV (Table 1). Our case and the review of the literature supports ultrasound evaluation for acute scrotal pain and swelling after laparoscopic appendectomy.
CONCLUSIONS
Scrotal abscess formation post-appendectomy is a rarely documented phenomenon. Although it occurs more commonly on the right side in the setting of a PPV, absence of a PPV and left sided occurrences have been reported. Thus, post-appendectomy scrotal pain and swelling, regardless of the affected side, warrants evaluation to rule out an intra-scrotal abscess.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



