-
PDF
- Split View
-
Views
-
Cite
Cite
Yahya Almarhabi, Asymptomatic cecal perforation and ileocecal fistula after intrauterine device migration: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 4, April 2020, rjaa015, https://doi.org/10.1093/jscr/rjaa015
Close - Share Icon Share
Abstract
Implantation of an intrauterine device (IUD) is a common method for long-term contraception. However, IUDs can cause colon perforation and fistula formation. We report a case of cecal perforation and ileocecal fistula secondary to IUD migration. The present study investigated incidental identification of a missing IUD after 9 years of deployment in a 35-year-old female with a three-year history of infertility. Abdominal imaging revealed a missing IUD. Intracecal perforation and ileocecal fistula consequent of IUD migration were identified during surgical exploration. Limited ileocecal resection was performed as an appropriate and safe surgical option. IUD migration can present with serious complications. Patients considering IUDs should be educated about the importance of regular check-ups to monitor the position of the IUD. Thorough examination should be carried out if a missing IUD string is reported.
INTRODUCTION
Intrauterine devices (IUDs) are a widely used and safe method of contraception. It is estimated that IUDs are used in around 9–14% of patients using long-term contraception worldwide [1, 2]. However, IUDs can present with rare complications such as uterine perforation, which occurs in approximately 1.3–1.6 cases per 1000 [1, 3].
This is a case of IUD perforation, intraluminal cecal perforation and ileocecal fistula. A literature review was carried out to assess the clinical presentation and management of IUD complications.
CASE REPORT
This was a 35-year-old married, multigravida female who was admitted to the Obstetrics and Gynaecology department of our institution for an elective exploration laparoscopy to retrieve a missed IUD. The patient was healthy otherwise. The patient’s obstetric history, an insertion of an IUD more than 9 years ago, was carried out at a private clinic. During a routine check-up 6 months after implantation, the IUD string had disappeared. A presumptive diagnosis of spontaneous expulsion was made. The patient underwent a new implantation of IUD, which was carried out at the same private clinic. The IUD was removed 2 years later. The patient has since had a successful pregnancy and the foetus was delivered by a Caesarean section (CS) 1 year after removal of the IUD. However, over the last 3 years, the patient has experienced difficulty conceiving. The patient has not experienced any complaints. During radiological tests, a foreign body in the right lower quadrant was detected by hysterosalpingogram. Based on these findings, laparoscopy exploration to retrieve the presumptive IUD was carried out.
On admission, the patient’s vital signs were normal. The patient was conscious and alert, with normal body-built habits. No anomalies were detected. No abdominal tenderness was observed. The results of her blood works were normal.
The patient underwent laparoscopic exploration. The obstetrics and gynaecology team were unable to locate the IUD in the free peritoneal cavity. However, the team identified adhesion at the level of the ileocecal junction and suspected a foreign body in the cecum with ileocecal fistula. The laparoscopic examination transitioned to an open laparotomy by route of the patient’s existing CS scar, and our team was called to carry out the procedure. A consent to carry out exploratory laparotomy was sought.
The laparotomy demonstrated that the IUD had penetrated the cecal wall through the base of the cecum. The IUD was palpated within the cecum (Fig. 1). The IUD was not fully mobile and was located approximately 8 cm from the appendix. In addition, ileocecal fistula was apparent between the terminal 7 cm of the ilium, and the entry point of the IUD at the base of the cecum (Fig. 2). A normal appendix was visualized at the base of the cecum (Fig. 3). Fibrosis in the uterine fundus was also observed. There were no other abnormalities to report.


Ileocecal fistula has been identified at the base of the cecum at the entry point of the migrated IUD.
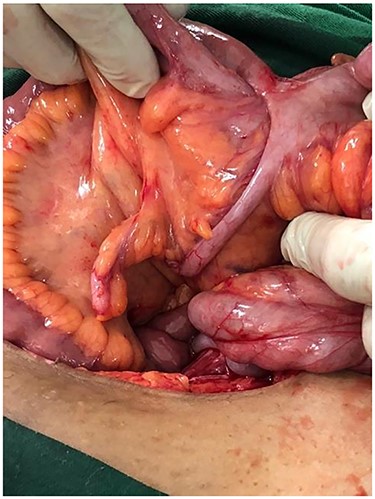
Normal appendix has been identified at a normal location and near to ileocecal fistula.
Given the immobility of the foreign body and ileocecal fistula, a limited ileocecal resection was performed with a side-to-side anastomosis. We identified the missed IUD in the resected specimen (Fig. 4). The patient was discharged on post-operative day three with follow-up in the clinic.

DISCUSSION
The IUD is considered a safe and reversible long-term contraception option. IUDs are inexpensive, which makes them a preferential contraceptive approach in developing countries when compared with developed countries (14.7 vs. 8.9%, respectively) [1, 4].
IUD expulsion is mostly reported with an incidence of up to 25% [1, 5]. After suspected IUD migration, a thorough gynaecological examination and radiological investigations should be performed [3, 6]. It is recommended that patients undergo a regular check-up to avoid possible IUD migration [1, 3, 4]. In this case study, the details of the presumptive diagnosis of IUD migration are not available; however, the second IUD implantation was carried out by the same medical staff that carried out the initial IUD insertion.
The risks associated with the use of IUDs include uterine bleeding, abortion and ectopic pregnancy [3]. Unwanted pregnancies have been observed in 30% of IUD users [3, 5]. IUDs present with rare but serious complications such as uterine perforation and migration of the IUD. The most involved organs are the omentum and gastrointestinal tract (GIT). Of the GIT, the sigmoid colon is the most commonly involved portion of the GIT (40.4%) [7]. In the present case study, the cecum was affected, which is very rare.
There are many risk factors of IUD penetration. These can be related to the IUD itself. Patient factors include the uterine anatomical configuration and the insertion period [1, 7]. The experience of the surgeon is another related factor [7]. In the present case study, the level of training of the surgeon who inserted the IUD is unknown. The patient demonstrated a normal uterine anatomy.
Migrated IUD is asymptomatic in 80% of cases [3, 6]. Possible symptoms include mild abdominal pain (53% of cases), vaginal bleeding and infertility. Acute intestinal obstruction or fistula has been reported as rare complications [1]. In the present case study, IUD migration was diagnosed accidently during an investigation into the patient’s inability to conceive for more than 3 years.
According to the World Health Organization and the International Federation for Family Planning, surgical removal of the IUD is recommended [8]. Accordingly, we decided to carry out surgical removal of the IUD in the present case study.
The surgical approaches to remove a migrated IUD vary. Laparoscopy exploration has been recommended as a first-line treatment, which has a success rate of between 40 and 100% [1, 9]. The endoscopy approach has been reported in cases of intraluminal colonic migration [8]. In the present case study, the procedure began with laparoscopy; however, due to the adhesion and risk of perforation, the surgical approach converted to open laparotomy. The IUD was intraluminal, but it was not fully mobile. In addition to ileocecal fistula and the adjacency of the appendix, surgery for limited ileocecal resection was carried out.
CONCLUSION
IUDs are effective contraceptive measures. Diagnosis of a migrated IUD should be based on a thorough gynaecological examination and appropriate radiological imaging approaches. Surgical removal is a first-line option to avoid serious complications.
Conflict of interest statement
The author declares that he has no conflict of interest.
Funding
This project was funded by the Deanship of Scientific Research (DSR) at King Abdulaziz University, Jeddah (Grant No. RG-3-140-38). The authors gratefully acknowledge the DSR for technical and financial support. The DSR had no role in the design of the study, data collection, data analysis, interpretation of data, or writing of the article.
ETHICAL APPROVAL
The study was approved by Ethics Committee of Aya Hospital.
AUTHOR CONTRIBUTIONS
Yahya Almarhabi-Data collection, editing of manuscript, drafting of manuscript, and literature review.
ACKNOWLEDGMENT
The author would like to thank Enago (www.enago.com) for the English language review.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.



