-
PDF
- Split View
-
Views
-
Cite
Cite
Yao C Huang, David Mitchell, Multiple concurrent complications of Roux-en-Y gastric bypass with MiniMizer gastric ring—alimentary limb intussusception through slipped ring into pouch, with remnant stomach internal herniation, Journal of Surgical Case Reports, Volume 2020, Issue 3, March 2020, rjaa033, https://doi.org/10.1093/jscr/rjaa033
Close - Share Icon Share
Abstract
Roux-en-Y gastric bypass (RYGB) is the second most common bariatric procedure performed in Australia, second to sleeve gastrectomy. Banding of pouches and anastomoses, via silastic bands or MiniMizer rings, have been used to assist in improving restriction. Though banded gastric bypasses are effective in weight loss, band migration, whether it be slippage or erosion, occurs in up to 7% of banded bariatric procedures. Jejunal intussusception and internal herniation are both individually known complications of RYGB. It is, however, rare to have all three phenomenon occur in a single patient. In this study, the authors present a report of a middle-aged lady, 2 years post-primary RYGB with MiniMizer gastric ring insertion presenting with all three complications.
INTRODUCTION
Roux-en-Y gastric bypass (RYGB) is the second most common bariatric procedure performed in Australia, second to sleeve gastrectomy. Banding of pouches and anastomoses, via silastic bands or MiniMizer rings, have been used to assist in improving restriction and reduce post-operative dumping syndrome [1]. As such, banded gastric bypasses are a frequently accepted variation and have been reported to improve weight loss and mitigate weight regain [1].
Though banded gastric bypasses are effective in weight loss [1], band migration, via slippage or erosion, can occur in up to 7% of cases [2, 3]. Jejunal intussusception and internal herniation are both individually known complications of RYGB. It is, however, rare to have all three phenomenon occur in a single patient. In this study, the authors present a report of a middle-aged lady, 2 years post-primary banded RYGB presenting with all three complications.
CASE REPORT
A 32-year-old female presented to our tertiary hospital with a 24-h history of sudden onset right and left upper quadrant pain in the setting of 2 days of increasing nausea, vomiting and inability to tolerate solids. This was on a background of being 18 months post-primary RYGB and MiniMizer gastric ring insertion performed privately.
Her original surgery was uncomplicated and she had experienced excellent weight loss, dropping from 148 kg pre-operatively, to 63 kg over the space of 18 months. Unfortunately, she had developed post-prandial vomiting intermittently for the last year and was in the process of undergoing work-up at our clinics. A barium swallow had demonstrated no abnormalities and she was due for an upper endoscopy.
On presentation, she was not obstipated and did not have any per rectal bleeding. Her pain was coliky and unrelated to food. She was a non-smoker, denied any recent change in diet and was only a recreational drinker. She had no other significant past medical or surgical history. On examination, her observations were within normal limits, she had a tender epigastrium but otherwise, a benign examination. Computer tomography demonstrated an intussusception (Fig. 1).

Computer tomography findings of alimentary limb jejunal intussusception into the gastric pouch, through the MiniMizer gastric ring.
The patient was positioned supine, and cut down entry periumbilically was performed with a 10-mm camera port and two 5-mm working ports inserted. On laparoscopy, a retrograde intussusception with the intussuscipien constituted the gastric pouch and the intussusceptum constituting the alimentary limb of the jejunum was identified. Just distal to the intussusceptum, there was a jejunal mesenteric defect, with demonstrable thinning of mesenteric fat and various tears. Through this defect, the remnant stomach, normally situated on the left side of the gastric pouch, was found to have herniated from the left to right through this jejunal mesenteric defect, posterior to the alimentary limb in the supracolic compartment. This internal hernia was reversed and the defect closed with non-dissolvable V-Loc™ barbed sutures. A slipped MiniMizer gastric ring was then identified 3 cm distal to the gastrojejunal anastomosis (Fig. 2). No fixation sutures were identified. On release of the ring, 25 cm of alimentary limb jejunum was, with gentle traction, pulled from its invagination into the gastric pouch through where the ring was originally placed (Fig. 3). Surprisingly, all bowel was viable and no resection was required.
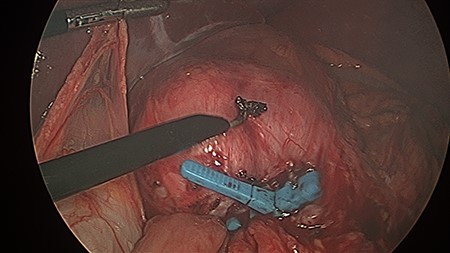
This figure demonstrates operative findings prior to surgical manipulation. The MiniMizer band is present at forefront, 3 cm distal to gastrojejunal anastomosis. The intussusception and internal herniation may be difficult to appreciate from this image.
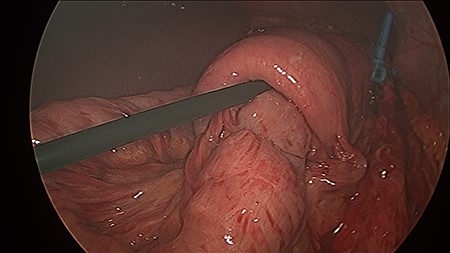
The MiniMizer ring has been removed. Alimentary limb jejunal intussusception and left to right remnant stomach herniation can be appreciated. Gentle traction on the intussusceptum resulted in 25 cm of viable bowel pulled from the invagination.
The patient was commenced on clear fluids day one post-operatively, upgraded to full diet the following day and was subsequently discharged Day 3 post-operatively. The patient experienced an uneventful recovery, receiving follow up in the first month and for a second time at the 6-month mark. She continues to be asymptomatic and has not required any further significant imaging.
DISCUSSION
The incidence, management and risk factors for retrograde intussusception and internal herniation are well documented in the literature. Retrograde intussusception in RYGB has an incidence of 0.1–0.6% and is commonly identified on CT [4]. Though still unclear, etiology is typically due to the formation of a lead point, typically a staple line though, as in this case, potentially the slipped MiniMizer band. Dysmotility from ectopic pacemaker cells has also been cited as a cause [4, 5]. Intussusception can be managed with simple reduction though this carries an 8–31.5% risk of recurrence [4]. Alternative options include reduction with plication, resection of affected bowel or resection and revision of the anastomotic lead point. The latter, carries a 7.7% risk of recurrence [4].
Internal hernias post RYGB have an incidence of 2–9% and are often due to surgically defects such as Petersen’s, jejunojenunal anastomosis or transverse mesocolon defect [6]. This carries a mortality of 1.6% and is generally related to loss of intraabdominal fat and surgical technique. Studies have demonstrated a significant reduction in internal hernias via routine closure of these defects with non-absorbable continuous sutures [6, 7]. Interestingly, our findings were not consistent with these common sites though we hypothesize that the mesenteric defect found may have been due to fat thinning and potentially traction.
Though the banded bypass is reported to improve weight loss, weight loss maintenance, delay gastric emptying and reduce post-operative dumping syndrome, a retrospective study of 1150 patients found no significant difference in weight loss after 2 or 3 years [3]. In contrast, another study did demonstrate a significant weight loss advantage to the banded groups but also stressed that both groups still achieved successful weight loss [1]. Though there was no significant difference in major post-operative complications, banded bypasses had a significantly increased risk of vomiting with up to 28% of patient reporting daily to weekly vomiting compared to 12% of non-banded bypasses [1, 8].
Banded bypasses also risk band migration. Silastic bands can erode in 0.9–7% of cases and can be managed expectantly, endoscopically or surgically [2, 3]. Though no erosion was observed in our case, distal slippage was found. This is rare, occurring in 1.5% of cases, and can potentially, as in our case, be due that the lack of fixation sutures or clips [9, 10].
We present this case to stimulate discussion on the potential risks involved in banding bypasses. We hope to highlight the potential rare, but extensive late complications that can occur simultaneously in a single patient years after their initial operation.
ACKNOWLEDGEMENTS
We acknowledge Dr George Hopkins for his referral of this patient to our care.
CONFLICTS OF INTEREST
None declared.
PERMISSIONS
The patient has given explicit consent to presenting this case, images and findings for purposes of education, publication and research.
References
Author notes
The authors are not recipients of research scholarships.



