-
PDF
- Split View
-
Views
-
Cite
Cite
Krishanth Naidu, Sivakumar Gananadha, An uncommon presentation of a sinister entity, Journal of Surgical Case Reports, Volume 2020, Issue 2, February 2020, rjz357, https://doi.org/10.1093/jscr/rjz357
Close - Share Icon Share
Abstract
A case of a female patient presenting with clinical findings ominous for a neoplastic bowel obstruction is reported. Abdominal computed tomography demonstrated a bowel obstruction with evidence of intussusception. Laparotomy revealed an irreducible ileoileal intussusception and segments of the jejunum infiltrated with pigmented deposits. There was no perforation and no evidence of an ulcerating or fungating mass. Intestinal melanoma is not an uncommon sequela of cutaneous melanoma, yet the disease can occur as a primary intestinal process, albeit this is a rarity. Surgical resection is the primary treatment modality and may offer the hope of increased symptom-free survival and overall survival for those patients suffering from metastatic or primary melanoma of the small intestine.
INTRODUCTION
Intestinal melanoma may arise as a primary or secondary neoplasm, although the former is rare. Most often the primary is a cutaneous lesion, but it may arise from anal or ocular sites. Constitutional symptoms may be present. Hematemesis and melena are not uncommon symptoms, but perforation is unusual. PET scan provides the most effective means for investigating suspected intestinal melanoma, but computed tomography (CT) scan is a real-world compromise. Surgical resection is the mainstay of treatment, but currently debate still exists regarding the curative potential of resection. Nevertheless, what is not doubted is the improvement in overall survival and symptomatic relief that comes with adequate resection.
CASE REPORT
A 47-year-old woman, who was previously well, presented with a 2-week history of worsening abdominal pain associated with vomiting. Weight loss of over 10 kg in 2 months was also reported. On physical examination she was afebrile, and abdominal examination revealed a distended and tender abdomen with a right lower quadrant mass.
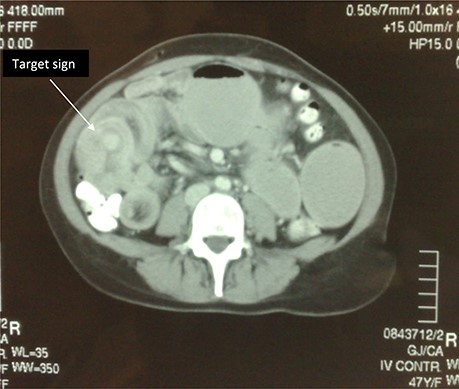
Subsequently she underwent radiological investigation of her chest and abdomen. CT abdomen revealed distension of the stomach as well as grossly distended loops of the small bowel. There was a lead point noted in the right iliac fossa with an ileoileal intussusception (Fig. 1). CT of her chest showed a large heterogeneous soft tissue density in the left upper lobe with associated left hilar and subcarinal lymphadenopathy.
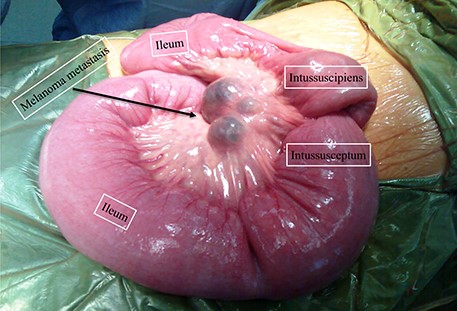
Findings at laparotomy demonstrating multiple pigmented lesions with ileoileal intussusception.
An emergency laparotomy was performed that confirmed an ileal intussusception, which was irreducible (Fig. 2). There were numerous small-to-moderate-sized pigmented deposits throughout the bowel and mesentery. A total of 40 cm of the jejunum and the corresponding mesentery with lymph nodes was removed. Histopathology confirmed metastatic melanoma with 6/6 mesenteric lymph nodes positive for metastatic disease. A staging CT brain showed two enhancing lesions in the right frontal and frontoparietal regions consistent with metastatic disease given her history. She was discharged home 10 days after laparotomy with plans for palliative treatment. The patient, however, died 2 months later.
DISCUSSION
Melanoma has long been known as the silent killer with rapid growth characteristics and a propensity to metastasize early to the brain, lungs, liver, and the gastrointestinal tract (GIT). While metastasis has been known to occur in nearly all GIT organs, it has a strong predilection for the small bowel with 58% of the total melanoma GIT metastases localizing to the small bowel [1, 2]. Intestinal melanoma can arise from cutaneous, anal, and ocular sites, but it may also occur as a primary small bowel tumor. Primary intestinal melanoma tends to occur in the ileum as a solitary intramucosal lesion, whereas secondary intestinal melanoma tends to arise in both the jejunum and ileum with multiple polypoid submucosal lesions [3]. The lesions may be ulcerated and crucially they may be amelanotic [3]. Intussusception is not an uncommon sequela of intestinal melanoma. Superficial spreading melanoma is the most common subtype of melanoma associated with intestinal metastasis, although this is most likely due its greater prevalence in the community [1].
Symptoms can be divided into obstructive (nausea, vomiting, abdominal pain, constipation), hematological (hematemesis and melena), and constitutional (anorexia, fatigue, weight loss) [3, 4, 5]. Patients may show physical signs of anemia and an abdominal mass may be present [5, 6]. Perforation is not usually a feature of this disease.
In terms of radiological investigations, positron emission tomography (PET) is superior to CT scanning for the detection of visceral metastases, with respective sensitivities of 100% and 69% [1, 3]. However, its clinical utility is somewhat negated by its limited availability in clinical practice. Other investigations include endoscopy, small bowel series, and ultrasound, although these investigations remain inadequate as a sole investigational tool.
Management must consider the clinical state of the patient, and the presence (and extent) of non-GIT disease. While important for palliation, the role of systemic therapies remains a constantly evolving field with surgical management remaining the mainstay modality [3]. Operative intervention primarily involves resection of the diseased segment with accompanying mesentery and lymph nodes, although in some cases other viscera such as the spleen or head of the pancreas may need to be sacrificed [4].
Sanki et al. found that survival rates were comparable with those of melanoma metastatectomy in other non-GIT organs, with the 5-year survival rate for intestinal melanoma approaching 27% [4]. Furthermore, regardless of its intent (curative or palliative), resection was associated with significant increases in overall survival and symptom-free survival [1, 4]. Considerable debate exists as to the curative capability of intestinal resection [3, 4]. Mean survival ranges from 28 to 48 months, although the median survival approaches 15 months [3, 4, 7].
†The corresponding author is not a recipient of a research scholarship.
‡This article is not based on a previous communication to a society or meeting.



