-
PDF
- Split View
-
Views
-
Cite
Cite
Christopher Seifen, Werner Herzig, Roger Schlüchter, Christian Schraner, A rare case of acute idiopathic colocolic intussusception in an adult patient, Journal of Surgical Case Reports, Volume 2020, Issue 12, December 2020, rjaa547, https://doi.org/10.1093/jscr/rjaa547
Close - Share Icon Share
Abstract
Adult intussusception is a rare condition that is frequently associated with malignancy and requires surgical approach. Symptoms are often non-specific and of subacute or chronic character. Therefore, computerized tomography (CT) scan is the most commonly used modality for identifying adult intussusception. A 51-year-old female presented with a 1-day history of increasing abdominal pain. Abdominal ultrasound and CT scan revealed intussusception. Intra-operatively, colocolic intussusception was present and laparoscopically reduced. A lead point was found neither intra-operatively nor in post-operative ileocolonoscopy and resection of involved bowel segments was not necessary.
INTRODUCTION
Intussusception is a condition where one part of the intestine is telescopically moved into a distal portion that affects the venous and subsequently the arterial blood flow. If left untreated, edema of the intestinal wall develops, followed by necrosis and the risk of perforation. Although intussusception typically occurs in children aged 4 months–2 years with a peak of incidence between 4 and 9 months of age [1], it is rarely seen in adults. We present a rare case of acute idiopathic colocolic intussusception in an adult patient.
CASE PRESENTATION
A 51-year-old female patient presented to the emergency department with abdominal pain that started and increased significantly within 1 day. The abdominal pain was described as crampy, appearing first in the periumbilical region with migration to the right lower quadrant. In addition, the patient experienced nausea, but no vomiting and had diarrhea twice that day without blood admixture. The patient’s past medical and family history were unremarkable. In physical examination, the abdomen was non-distended and soft but with rebound tenderness, especially in the right lower and middle quadrant. The rectum was empty and there was no indicator of intestinal hemorrhage. Laboratory tests showed a white blood cell count of 14.5 × 109/L and a C-reactive protein level of 7.0 mg/L. All other studies were within normal limits. An abdominal ultrasound showed a ‘pseudokidney’ sign in the lower abdomen (Fig. 1). Additionally, a computerized tomography (CT) scan of the abdomen and pelvis was performed and revealed an intussusception involving ~20 cm of the ascending and transverse colon (Fig. 2).
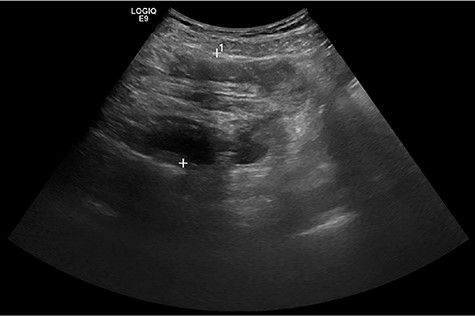
Abdominal ultrasound showed a ‘pseudokidney’ sign on the longitudinal view of the lower abdomen.
The patient was urgently taken to the operating room with a pre-operative diagnosis of colon intussusception and underwent laparoscopy. Intra-operatively, colocolic intussusception was present. The cecum was found to be the intussusceptum, subsequently telescoping far into the transverse colon that was found to be the intussuscipiens (Fig. 3).
The intussusception was reduced successfully by milking it out in a distal to proximal direction from outside. No other lesions, especially no lead point, were found during laparoscopy. The colon showed no signs of necrosis or damage. The post-operative course was uneventful. An additional ileocolonoscopy was performed on the third day after surgery. The cecum presented mucosal alterations, whereas the terminal ileum and the remaining colon showed normal mucosa. Biopsies of the cecum showed intact mucosa without histological features of ischemic injury. In addition, no signs of dysplasia or malignancy were found. The patient was discharged on the fourth day after surgery in good state of health. A second ileocolonoscopy was performed 8 weeks after the intussusception: The cecum and the appendix appeared to be prolonged, whereas no further abnormal features could be found. We decided for laparoscopic cecopexy and appendectomy that was performed 12 weeks after the intussusception. During follow-up, the patient showed no recurrence and fully recovered.
DISCUSSION
Intussusception was first described by Paul Barbette of Amsterdam in 1674 [2] and first operated on successfully by John Hutchinson in 1873 [3]. In 1956, Dean et al. classified intussusception in adults according to its location as enteric (43%), colocolic (22%), ileocecal (21%) and ileocolic (14%) [4]. Intussusception can occur at any age but is mostly seen in the pediatric population. In infants, the majority of cases have no lead point and are classified as primary or idiopathic intussusceptions [5]. Primary or idiopathic intussusception in adults accounts only for ~8–20% of all cases. In contrast, secondary intussusception associated with a pathological condition involving a lead point is more commonly present in adult population [6]. Lead points for secondary intussusception can be multiple, e.g. Meckel’s diverticulum, polyps, adhesions after abdominal surgery or malignancies. A malignant etiology accounts for ~30% of small-bowel intussusception and 66% of large bowel intussusception. The clinical presentation of intussusception varies considerably. The classic triad of cramping abdominal pain, bloody diarrhea and a palpable mass is frequently seen in the pediatric population. However, in adult population, the classic triad is often absent. Mostly, symptoms are non-specific and cases have been reported as acute, subacute and chronic. Therefore, diagnosis in adult population is more challenging and frequently requires diagnostic imaging [7]. Abdominal ultrasound is considered a useful tool for the diagnosis of intussusception in both children and adults, presenting a ‘target’ or ‘doughnut’ sign on the transverse view and a ‘pseudokidney’ or ‘hayfork’ sign on the longitudinal view. Despite its high sensitivity and specificity, diagnostic accuracy can be limited by obesity, massive air in the bowel or an unexperienced examiner [8]. Furthermore, abdominal CT scan is the most commonly used modality with high sensitivity and specificity. When intussusception is present, a ‘target’ or ‘sausage’-shaped lesion can be seen [9]. Additionally, CT scan of the abdomen may help to find a lead point causing a secondary intussusception or may help to stage the patient when a suspected malignancy is present [7]. Due to the high incidence of malignancy or other structural change causing adult intussusception, a surgical approach traditionally has been served as the treatment of choice [7]. However, the extent of surgery is widely discussed and remains controversial. For example, bowel resection following oncologic principles is recommended in elderly patients with colonic intussusception based on the high incidence of underlying malignancy. In such case, most authors suggest en bloc resection without reduction of the intussusception due to the risk of tumor spillage [6]. In contrast, newer studies considered non-operative management in adult enteric intussusception that is shorter than 3.5 cm due to its often self-limiting nature [10]. In pediatric population, intussusception is commonly reduced non-surgically with barium or air [5].

Intravenous contrast-enhanced abdominal and pelvic CT scan showed the full extent of the colocolic intussusception. No lead point was evident. (Left) Coronar view with ‘sausage’-shaped lesion. (Middle) Axial view with ‘sausage’-shaped lesion. (Right) Sagittal view with ‘targed’-shaped lesion.
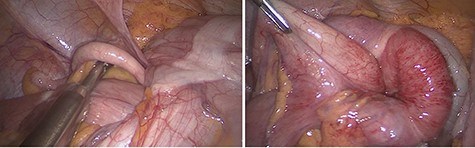
Intra-operative finding of the intussusception. (Left) The terminal ileum and the appendix were pulled like a tail by the intussusceptum into the intussusception. (Right) The cecum was identified as the intussusceptum, telescoping into the transverse colon that was identified as the intussuscipiens.
In the present case, laparoscopy was performed to reduce the intussusception by milking it out in a distal to proximal direction. Because a lead point could not be found in pre-operative CT scan, intra-operatively or in post-operative ileocolonoscopy, a bowel resection was not necessary. This decision was supported by acute onset of complaints and lacking B symptoms.
The presented case offers a combination of four unlikely features that makes it rare: (i) manifestation in an adult; (ii) presentation of acute clinical symptoms; (iii) colocolic localization and (iv) missing indication of a lead point.
INFORMED CONSENT
The patient has consented for this case report to be published.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



