-
PDF
- Split View
-
Views
-
Cite
Cite
Ekta Paw, Chelsea T W Ong, Venkat Vangaveti, Pott’s puffy tumour in an immunosuppressed adult: case report and systematic review of literature, Journal of Surgical Case Reports, Volume 2020, Issue 12, December 2020, rjaa528, https://doi.org/10.1093/jscr/rjaa528
Close - Share Icon Share
Abstract
This case is of a 34-year-old immunocompromised male with Pott’s puffy tumour, which was treated with antibiotics and endoscopic sinus surgery. Pott’s puffy tumour is typically a complication of frontal sinusitis in children and immunocompromise can be a precipitating factor.
A search was conducted of Embase, Medline, CINAHL, Cochrane, Google Scholar, Informit and Scopus of ‘Pott’s Puffy’ and variations of this phrase. Initial 804 records were reviewed by title, abstract and full text.
Of the unique papers identified, 155 only included paediatric patients and 128 included adult patients. After title, abstract and full-text review of 13 papers were identified describing Pott’s puffy tumour in immunocompromised patients.
Immunosuppression was noted as a risk factor in only a small number of cases, with diabetes mellitus being the most common. A few cases did note immunosuppression due to newer immunomodulatory agents being used for treatment of autoimmune conditions.
INTRODUCTION
This case is of a 34-year-old immunosuppressed male who presented with Pott’s puffy tumour as a complication of frontal sinusitis. Surgical incision and drainage was performed with endoscopic debridement of sinuses, in addition to treatment with antibiotics and nasal decongestants. This case highlights immunosuppression, particularly with tumour necrosis factor (TNF) inhibitors, as a potential risk factor for development of Pott’s puffy tumour as a complication of frontal sinusitis.
CASE REPORT
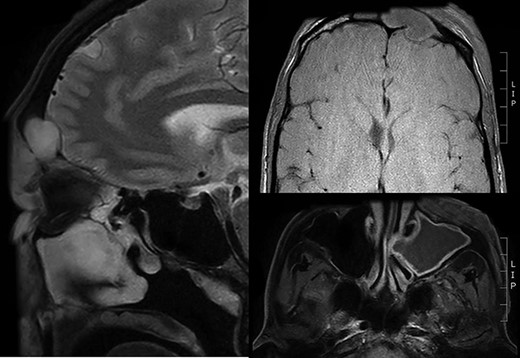
A 34-year-old gentleman presented to the emergency department of a regional hospital with 2 days of left-sided periorbital swelling superior to the eye socket with associated erythema and tenderness. He was assessed to have normal visual acuity and extraocular movements. He had a history of severe ankylosing spondylitis for which he was taking a TNF inhibitor, adalimumab. His blood tests showed a slightly raised C-reactive protein of 82 mg/l but otherwise no abnormality. Magnetic resonance imaging (MRI) was performed on the day of admission and noted significant left frontal sinusitis complicated by a defect of the frontal cortical bone as well as oedema and enhancement consistent with a Pott’s puffy tumour (Fig. 1). There was also an abscess of the periorbital soft tissue. Immediate treatment was given in the form of phenylephrine nasal decongestants and intravenous antibiotics (amoxicillin with clavulanic acid), and the patient was transferred to a tertiary centre with ear, nose and throat surgery capacity.
Within 24 hours of arrival at the tertiary centre, an incision and drainage of the soft tissue abscess and periosteal abscess was performed. At the same time the sinuses were debrided via endoscopic approach and a wide maxillary antrostomy and sphenoidectomy was performed. It was discovered that the frontal recess was completely occluded by a bony wall (Fig. 2). A cannula was placed into the frontal sinus for regular irrigation during the post-operative period with the other sinuses irrigated via nasal douche. Intravenous antibiotics and regular irrigation were continued for a further 5 days, and the TNF inhibitor was withheld on the advice of a rheumatologist. After this time the frontal sinus cannula was removed and the patient was discharged home. He was reviewed as an outpatient 6 days later and had a palpable soft tissue collection in the same area, which was promptly drained surgically and appeared to be a mucocele intraoperatively. None of the cultures identified a specific causative organism, although a Gram stain from the original admission showed gram negative bacilli. The patient was planned to have definitive surgery to open the bony occlusion of the frontal sinus and allow proper drainage. The patient was noted not to have any recurrence of symptoms on follow-up 1 year post-operatively.
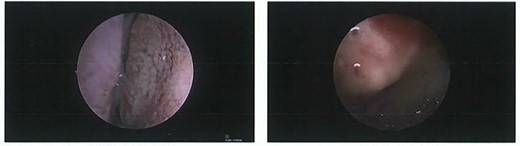
Intraoperative photos. Left: view of dura on endoscopic examination of frontal sinus via bony erosion. Right: complete bony occlusion of frontal recess
Summary of all cases Pott’s puffy tumour cases found with immunosuppression of patients
| Author . | Age . | Sex . | Presenting complaint . | Immunocompromised . | Intracranial spread . | Pathogen . | Surgical management . | Complications . |
|---|---|---|---|---|---|---|---|---|
| Adams et al. [5] | 55 | M | Pain, swelling, watery discharge | Diabetes mellitus | Left meningeal abscess | Pseudomonas aeruginosa | Bilateral frontal balloon catheter sinustomy, bilateral complete ethmoidectomy, bilateral middle meatal antrostomy, right sphenoidectomy | Chronic ethmoid sinusitis and left orbital abscess requiring surgery |
| Akiyama et al. [6] | 21–83 | M + F | Diabetes, chronic renal failure, aplastic anaemia, breast cancer with bone metastasis | — | — | External (58.1%) or endoscopic (32.9%) frontal sinus surgery, frontal bone debridement, craniotomy, simple percutaneous drainage (9.7%) | 2 cases of postoperative recurrence | |
| Chow and Szeto [7] | 60 | F | Headache, swelling, fever, peritonitis | End stage renal failure | — | Mycobacterium tuberculosis | — | — |
| Domville-Lewis et al. [8] | 21 | F | Headache, swelling, chemosis | Pregnancy | Right epidural empyema posterior to frontal sinus | Streptococcus milleri | Percutaneous drainage, unilateral ucinectomy, middle meatal antrostomy, anterior ethmoidectomy, frontal recess dissection | Caesarean section |
| Effat et al. [9] | 62 | F | Headache, swelling, fever, purulent, discharge | Insulin-dependent diabetes, chronic renal failure on twice weekly haemodialysis | Erosion of lamina papyracea of left anterior and middle ethmoid cells and subperiosteal abscess | Mucorales | Cruciate incision and drainage, daily debridement | Fistula |
| Evliyaoǧlu et al. [10] | 27 | M | Pain headache, swelling, fever | Type 1 diabetes mellitus | Subperiosteal abscess in vertex region associated with dural thickening and irregularities of epidural space | — | Bicoronal skin incision under local, drainage of subperiosteal abscess, curette | — |
| Gil-Carcedo et al. [11] | 48 | M | Left hemiparesis, neck stiffness, right mydriasis, confusion, seizure | Chronic alcoholism | Epidural abscess, subdural empyema | Unclassified aerobic streptococcus | Right frontoparietal craniotomy, intraoral antrostomy and bilateral transantral ethmoidectomy, reconstruction with acrylic grafts | — |
| Goldfarb et al. [12] | 58 | M | Pain, swelling | Heavy smoking, diabetes mellitus | — | — | Incision and drainage | Fistula between frontal sinus and forehead skin |
| Husta and Reichner [13] | 43 | M | Altered mental status, proptosis | HIV, cocaine abuse | Subdural empyema, intracranial abscesses resulting in midline shift | Streptococcus mitis | Drainage of the right frontal subperiosteal abscess, left temporal craniotomy and evacuation of subdural empyema | Hypoxaemic respiratory failure requiring intubation, multiple bilateral cavitary lung abscess in bases |
| Lamoreau and Fanciullo [14] | 55 | M | Left eye abscess, fever | Alcoholic cirrhosis, hepatitis C, nicotine, marijuana/other drug use | Left frontal bony erosion | Viridans like streptococci | Incision and drainage | Increased petit mal symptoms of known epilepsy |
| Miller [15] | 60 | M | Headache, swelling | Diabetes mellitus, prednisolone (weaning dose for allergy) | Erosion of anterior frontal sinus with posterior extension to meninges | Streptococcus anginosus | Spontaneously ruptured in hospital | — |
| Pasin et al. [16] | 81 | M | Painless swelling, weight loss, profound asthenia | Diabetes mellitus | Erosion of left frontal bone and orbital roof | Streptococcus constellatus | Endoscopic sinus surgery | — |
| Sekine et al. [17] | 56 | M | Headache, recurrent forehead swelling, eyelid erythema | Rheumatoid arthritis, treatment (prednisolone, iguratimod, bucillamine) | — | Stenotrophomonas maltophilia, Achromobacter xylosoxidans and Corynebacterium spp. | Bicoronal incision and endoscopic approach for drainage. Anterolateral thigh flap reconstruction. Revision of forehead cavity with titanium plate later. | — |
| Author . | Age . | Sex . | Presenting complaint . | Immunocompromised . | Intracranial spread . | Pathogen . | Surgical management . | Complications . |
|---|---|---|---|---|---|---|---|---|
| Adams et al. [5] | 55 | M | Pain, swelling, watery discharge | Diabetes mellitus | Left meningeal abscess | Pseudomonas aeruginosa | Bilateral frontal balloon catheter sinustomy, bilateral complete ethmoidectomy, bilateral middle meatal antrostomy, right sphenoidectomy | Chronic ethmoid sinusitis and left orbital abscess requiring surgery |
| Akiyama et al. [6] | 21–83 | M + F | Diabetes, chronic renal failure, aplastic anaemia, breast cancer with bone metastasis | — | — | External (58.1%) or endoscopic (32.9%) frontal sinus surgery, frontal bone debridement, craniotomy, simple percutaneous drainage (9.7%) | 2 cases of postoperative recurrence | |
| Chow and Szeto [7] | 60 | F | Headache, swelling, fever, peritonitis | End stage renal failure | — | Mycobacterium tuberculosis | — | — |
| Domville-Lewis et al. [8] | 21 | F | Headache, swelling, chemosis | Pregnancy | Right epidural empyema posterior to frontal sinus | Streptococcus milleri | Percutaneous drainage, unilateral ucinectomy, middle meatal antrostomy, anterior ethmoidectomy, frontal recess dissection | Caesarean section |
| Effat et al. [9] | 62 | F | Headache, swelling, fever, purulent, discharge | Insulin-dependent diabetes, chronic renal failure on twice weekly haemodialysis | Erosion of lamina papyracea of left anterior and middle ethmoid cells and subperiosteal abscess | Mucorales | Cruciate incision and drainage, daily debridement | Fistula |
| Evliyaoǧlu et al. [10] | 27 | M | Pain headache, swelling, fever | Type 1 diabetes mellitus | Subperiosteal abscess in vertex region associated with dural thickening and irregularities of epidural space | — | Bicoronal skin incision under local, drainage of subperiosteal abscess, curette | — |
| Gil-Carcedo et al. [11] | 48 | M | Left hemiparesis, neck stiffness, right mydriasis, confusion, seizure | Chronic alcoholism | Epidural abscess, subdural empyema | Unclassified aerobic streptococcus | Right frontoparietal craniotomy, intraoral antrostomy and bilateral transantral ethmoidectomy, reconstruction with acrylic grafts | — |
| Goldfarb et al. [12] | 58 | M | Pain, swelling | Heavy smoking, diabetes mellitus | — | — | Incision and drainage | Fistula between frontal sinus and forehead skin |
| Husta and Reichner [13] | 43 | M | Altered mental status, proptosis | HIV, cocaine abuse | Subdural empyema, intracranial abscesses resulting in midline shift | Streptococcus mitis | Drainage of the right frontal subperiosteal abscess, left temporal craniotomy and evacuation of subdural empyema | Hypoxaemic respiratory failure requiring intubation, multiple bilateral cavitary lung abscess in bases |
| Lamoreau and Fanciullo [14] | 55 | M | Left eye abscess, fever | Alcoholic cirrhosis, hepatitis C, nicotine, marijuana/other drug use | Left frontal bony erosion | Viridans like streptococci | Incision and drainage | Increased petit mal symptoms of known epilepsy |
| Miller [15] | 60 | M | Headache, swelling | Diabetes mellitus, prednisolone (weaning dose for allergy) | Erosion of anterior frontal sinus with posterior extension to meninges | Streptococcus anginosus | Spontaneously ruptured in hospital | — |
| Pasin et al. [16] | 81 | M | Painless swelling, weight loss, profound asthenia | Diabetes mellitus | Erosion of left frontal bone and orbital roof | Streptococcus constellatus | Endoscopic sinus surgery | — |
| Sekine et al. [17] | 56 | M | Headache, recurrent forehead swelling, eyelid erythema | Rheumatoid arthritis, treatment (prednisolone, iguratimod, bucillamine) | — | Stenotrophomonas maltophilia, Achromobacter xylosoxidans and Corynebacterium spp. | Bicoronal incision and endoscopic approach for drainage. Anterolateral thigh flap reconstruction. Revision of forehead cavity with titanium plate later. | — |
Summary of all cases Pott’s puffy tumour cases found with immunosuppression of patients
| Author . | Age . | Sex . | Presenting complaint . | Immunocompromised . | Intracranial spread . | Pathogen . | Surgical management . | Complications . |
|---|---|---|---|---|---|---|---|---|
| Adams et al. [5] | 55 | M | Pain, swelling, watery discharge | Diabetes mellitus | Left meningeal abscess | Pseudomonas aeruginosa | Bilateral frontal balloon catheter sinustomy, bilateral complete ethmoidectomy, bilateral middle meatal antrostomy, right sphenoidectomy | Chronic ethmoid sinusitis and left orbital abscess requiring surgery |
| Akiyama et al. [6] | 21–83 | M + F | Diabetes, chronic renal failure, aplastic anaemia, breast cancer with bone metastasis | — | — | External (58.1%) or endoscopic (32.9%) frontal sinus surgery, frontal bone debridement, craniotomy, simple percutaneous drainage (9.7%) | 2 cases of postoperative recurrence | |
| Chow and Szeto [7] | 60 | F | Headache, swelling, fever, peritonitis | End stage renal failure | — | Mycobacterium tuberculosis | — | — |
| Domville-Lewis et al. [8] | 21 | F | Headache, swelling, chemosis | Pregnancy | Right epidural empyema posterior to frontal sinus | Streptococcus milleri | Percutaneous drainage, unilateral ucinectomy, middle meatal antrostomy, anterior ethmoidectomy, frontal recess dissection | Caesarean section |
| Effat et al. [9] | 62 | F | Headache, swelling, fever, purulent, discharge | Insulin-dependent diabetes, chronic renal failure on twice weekly haemodialysis | Erosion of lamina papyracea of left anterior and middle ethmoid cells and subperiosteal abscess | Mucorales | Cruciate incision and drainage, daily debridement | Fistula |
| Evliyaoǧlu et al. [10] | 27 | M | Pain headache, swelling, fever | Type 1 diabetes mellitus | Subperiosteal abscess in vertex region associated with dural thickening and irregularities of epidural space | — | Bicoronal skin incision under local, drainage of subperiosteal abscess, curette | — |
| Gil-Carcedo et al. [11] | 48 | M | Left hemiparesis, neck stiffness, right mydriasis, confusion, seizure | Chronic alcoholism | Epidural abscess, subdural empyema | Unclassified aerobic streptococcus | Right frontoparietal craniotomy, intraoral antrostomy and bilateral transantral ethmoidectomy, reconstruction with acrylic grafts | — |
| Goldfarb et al. [12] | 58 | M | Pain, swelling | Heavy smoking, diabetes mellitus | — | — | Incision and drainage | Fistula between frontal sinus and forehead skin |
| Husta and Reichner [13] | 43 | M | Altered mental status, proptosis | HIV, cocaine abuse | Subdural empyema, intracranial abscesses resulting in midline shift | Streptococcus mitis | Drainage of the right frontal subperiosteal abscess, left temporal craniotomy and evacuation of subdural empyema | Hypoxaemic respiratory failure requiring intubation, multiple bilateral cavitary lung abscess in bases |
| Lamoreau and Fanciullo [14] | 55 | M | Left eye abscess, fever | Alcoholic cirrhosis, hepatitis C, nicotine, marijuana/other drug use | Left frontal bony erosion | Viridans like streptococci | Incision and drainage | Increased petit mal symptoms of known epilepsy |
| Miller [15] | 60 | M | Headache, swelling | Diabetes mellitus, prednisolone (weaning dose for allergy) | Erosion of anterior frontal sinus with posterior extension to meninges | Streptococcus anginosus | Spontaneously ruptured in hospital | — |
| Pasin et al. [16] | 81 | M | Painless swelling, weight loss, profound asthenia | Diabetes mellitus | Erosion of left frontal bone and orbital roof | Streptococcus constellatus | Endoscopic sinus surgery | — |
| Sekine et al. [17] | 56 | M | Headache, recurrent forehead swelling, eyelid erythema | Rheumatoid arthritis, treatment (prednisolone, iguratimod, bucillamine) | — | Stenotrophomonas maltophilia, Achromobacter xylosoxidans and Corynebacterium spp. | Bicoronal incision and endoscopic approach for drainage. Anterolateral thigh flap reconstruction. Revision of forehead cavity with titanium plate later. | — |
| Author . | Age . | Sex . | Presenting complaint . | Immunocompromised . | Intracranial spread . | Pathogen . | Surgical management . | Complications . |
|---|---|---|---|---|---|---|---|---|
| Adams et al. [5] | 55 | M | Pain, swelling, watery discharge | Diabetes mellitus | Left meningeal abscess | Pseudomonas aeruginosa | Bilateral frontal balloon catheter sinustomy, bilateral complete ethmoidectomy, bilateral middle meatal antrostomy, right sphenoidectomy | Chronic ethmoid sinusitis and left orbital abscess requiring surgery |
| Akiyama et al. [6] | 21–83 | M + F | Diabetes, chronic renal failure, aplastic anaemia, breast cancer with bone metastasis | — | — | External (58.1%) or endoscopic (32.9%) frontal sinus surgery, frontal bone debridement, craniotomy, simple percutaneous drainage (9.7%) | 2 cases of postoperative recurrence | |
| Chow and Szeto [7] | 60 | F | Headache, swelling, fever, peritonitis | End stage renal failure | — | Mycobacterium tuberculosis | — | — |
| Domville-Lewis et al. [8] | 21 | F | Headache, swelling, chemosis | Pregnancy | Right epidural empyema posterior to frontal sinus | Streptococcus milleri | Percutaneous drainage, unilateral ucinectomy, middle meatal antrostomy, anterior ethmoidectomy, frontal recess dissection | Caesarean section |
| Effat et al. [9] | 62 | F | Headache, swelling, fever, purulent, discharge | Insulin-dependent diabetes, chronic renal failure on twice weekly haemodialysis | Erosion of lamina papyracea of left anterior and middle ethmoid cells and subperiosteal abscess | Mucorales | Cruciate incision and drainage, daily debridement | Fistula |
| Evliyaoǧlu et al. [10] | 27 | M | Pain headache, swelling, fever | Type 1 diabetes mellitus | Subperiosteal abscess in vertex region associated with dural thickening and irregularities of epidural space | — | Bicoronal skin incision under local, drainage of subperiosteal abscess, curette | — |
| Gil-Carcedo et al. [11] | 48 | M | Left hemiparesis, neck stiffness, right mydriasis, confusion, seizure | Chronic alcoholism | Epidural abscess, subdural empyema | Unclassified aerobic streptococcus | Right frontoparietal craniotomy, intraoral antrostomy and bilateral transantral ethmoidectomy, reconstruction with acrylic grafts | — |
| Goldfarb et al. [12] | 58 | M | Pain, swelling | Heavy smoking, diabetes mellitus | — | — | Incision and drainage | Fistula between frontal sinus and forehead skin |
| Husta and Reichner [13] | 43 | M | Altered mental status, proptosis | HIV, cocaine abuse | Subdural empyema, intracranial abscesses resulting in midline shift | Streptococcus mitis | Drainage of the right frontal subperiosteal abscess, left temporal craniotomy and evacuation of subdural empyema | Hypoxaemic respiratory failure requiring intubation, multiple bilateral cavitary lung abscess in bases |
| Lamoreau and Fanciullo [14] | 55 | M | Left eye abscess, fever | Alcoholic cirrhosis, hepatitis C, nicotine, marijuana/other drug use | Left frontal bony erosion | Viridans like streptococci | Incision and drainage | Increased petit mal symptoms of known epilepsy |
| Miller [15] | 60 | M | Headache, swelling | Diabetes mellitus, prednisolone (weaning dose for allergy) | Erosion of anterior frontal sinus with posterior extension to meninges | Streptococcus anginosus | Spontaneously ruptured in hospital | — |
| Pasin et al. [16] | 81 | M | Painless swelling, weight loss, profound asthenia | Diabetes mellitus | Erosion of left frontal bone and orbital roof | Streptococcus constellatus | Endoscopic sinus surgery | — |
| Sekine et al. [17] | 56 | M | Headache, recurrent forehead swelling, eyelid erythema | Rheumatoid arthritis, treatment (prednisolone, iguratimod, bucillamine) | — | Stenotrophomonas maltophilia, Achromobacter xylosoxidans and Corynebacterium spp. | Bicoronal incision and endoscopic approach for drainage. Anterolateral thigh flap reconstruction. Revision of forehead cavity with titanium plate later. | — |
DISCUSSION
Pott’s puffy tumour is a rare clinical entity and is most commonly a complication of frontal sinusitis in children [1]. This case is unique in that it presents in an adult with no traumatic history and immunosuppression as the only risk factor. TNF inhibitors do not appear to have a significant association with sinusitis but due to being immunosuppressants may slightly increase the risk of upper respiratory tract infections [2]. A literature review was conducted to investigate the role of immunosuppression in Pott’s puffy tumour patients.
A search was conducted on 10 March 2020 of CINAHL, Cochrane Embase, Informit, Google Scholar (first 50 results only), Medline and Scopus of ‘Pott’s Puffy’ and variations of this phrase. Initial 804 records were reviewed by title, abstract and full text (as detailed in Fig. 3) and narrowed down to 13 papers of adult Pott’s puffy tumour where immunosuppression was noted in the case.
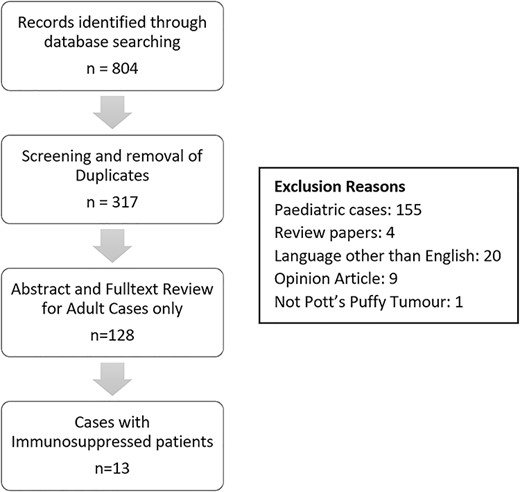
Of the unique papers identified, 155 only included paediatric patients, whereas 128 included adult patients. This would indicate that Pott’s puffy tumour in adult patients is not quite as rare as previously thought. The paediatric cases were reviewed by abstract only for immunosuppression and only four were found. Two girls also on the same immunosuppressant medication as this patient (TNF inhibitor adalimumab) developed Pott’s puffy tumour [3]. Another case of a 14 year old on an immunosuppressive study drug for juvenile idiopathic arthritis was published in the USA [4]. Finally one child with Type 2 diabetes mellitus in a case series was diagnosed with Pott’s puffy tumour [1].
Of the 13 adult patients’ papers comprising of both case reports and case series, 12 patients were immunosuppressed and 1 was pregnant (Table 1). The most commonly noted was diabetes in seven patients, and there was one patient with rheumatoid arthritis being treated with oral prednisolone, iguratimod and bucillamine.
Most Pott’s puffy tumour cases appear to be in previously fit and well patients, so immunosuppression may play less of a role than neglect of symptoms and delayed clinical review. In this patient the location being several hours drive from the nearest hospital may be more relevant than their immunosuppression. Nonetheless, a higher index of suspicion for severe complications of sinusitis should still be considered for immunosuppressive patients.
ETHICS APPROVAL
LNR/QTHS/67480.
CONFLICT OF INTEREST STATEMENT
None declared.



