-
PDF
- Split View
-
Views
-
Cite
Cite
Rachel W Davis, Youmna A Sherif, Catherine Anne Morrison, External stoma diversion: a palliative measure for peristomal wound healing in resource-limited settings, Journal of Surgical Case Reports, Volume 2020, Issue 12, December 2020, rjaa502, https://doi.org/10.1093/jscr/rjaa502
Close - Share Icon Share
Abstract
The provision of intestinal stoma care is challenging in austere settings due to limitations in surgical and wound care access as well as the high cost and sparsity of ostomy supplies. As a result, many surgical patients suffer from ostomy-related complications such as peristomal wounds and are unable to find relief for these complications from standard treatments and measures. This article describes the external stoma diversion, a cost-effective palliative surgical procedure that assists in the healing of peristomal wounds in resource-limited settings.
INTRODUCTION
Successful creation and maintenance of intestinal stomas requires strategic perioperative planning, adequate patient nutrition, thorough educational resources for patients and caregivers and ready access to postoperative wound care and supplies. A deficiency in any of these areas may present with significant complications including peristomal wounds, hernias, stenosis, retraction and ileus [1]. Peristomal wounds are the most common complication of ostomies. This is particularly true of ileostomies as they result in skin maceration much more often due to the higher acidity, higher concentration of corrosive enzymes and higher output volume. The result is a painful wound that increases nutritional burden in an already malnourished patient, and leads to a vicious cycle in which traditional adhesives fail and ongoing maceration continues. Peristomal wounds have, in turn, inspired an entire field of wound care and stimulated innovation in ostomy supplies and appliances [1]. While the creation of an intestinal stoma is often a lifesaving procedure, it is always a life-changing procedure as patients learn to appropriately manage their ostomies and cope with social ramifications.
There is an added layer of complexity for ostomy care in resource-limited settings. Patients often have difficulty accessing surgery for ostomy reversal due to travel required to reach tertiary care centers and the high costs associated with both travel and surgical care [2]. In the interim, patients may have limited access to traditional supplies, and must refashion common items into ostomy appliances and bags (e.g. using food bags, jar lids, cloth belts) [3]. Research has illustrated the adverse clinical outcomes associated with extended ostomy duration in contexts with insufficient access to ostomy supplies, education or care including peristomal skin complications [4]. Therefore, appropriate interventions for addressing peristomal wound in resource-limited settings is an imperative that can significantly improve a patient’s quality of life. This article describes an external stoma diversion performed at a district hospital in Tanzania as a palliative measure to assist in the healing of significant skin maceration resulting from a high-output end ileostomy.
CASE REPORT: DESCRIPTION OF EXTERNAL STOMA DIVERSION
Overview
The external stoma diversion is a cost-effective, palliative surgical procedure intended to assist in the healing of peristomal wounds. It is a temporizing measure that diverts stoma output into a collecting system through a waterproof conduit. The conduit is intended to be in place for ~1 week and serves as a viable adjunct for the palliation and treatment of significant peristomal wounds that have failed all standard treatments and measures.
Surgical procedure
The stoma site and surrounding skin are prepped with betadine and the area draped with sterile towels. While this is not inherently a sterile procedure, effort should be taken to minimize contamination. A condom is dropped from the packaging onto the field and unrolled. The distal end is cut to remove the reservoir, such that both ends of the condom are open and form a conduit. Local anesthetic, such as lidocaine without epinephrine, is then administered subcutaneously around the stoma.
The reinforced, proximal end of the condom is placed on the skin around the perimeter of the stoma. Using a permanent suture, the ring of the condom is then sewn to the skin immediately surrounding the stoma edge. We recommend using a 4.0 nylon suture on a cutting needle. The nylon is then run in a continuous fashion from 12:00 to 6:00 position and then tied. A second nylon is used to run the remaining half circle from 6:00 back to 12:00, and also tied (Fig. 1). Distal open end of the condom is then carefully secured to the uncapped collar of a plastic water bottle using a rubber band. This is most readily done by looping the rubber band around the mouth of the bottle prior to condom attachment, then extending it to place the condom edge beneath. The top edge of the bottle must be pierced with a large bore needle to allow air to escape as the bottle fills (Figs 2 and 3). The drainage system can then be secured to the patient’s waist using any cloth holster.
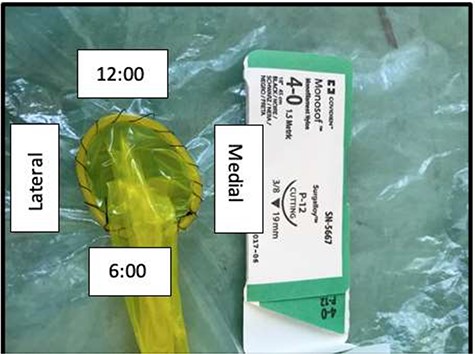
Orientation of external stoma diversion: the image shows a model of the external stoma diversion and its orientation, with the most cephalad point at 12:00 and most caudad point at 6:00.
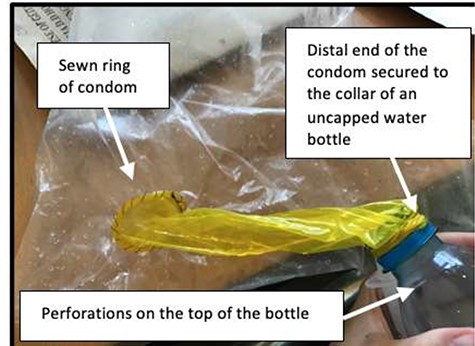
External stoma diversion prototype: this image shows a prototype, in which the condom ring is sewn around the stoma (here represented by a plastic bag) and the distal end divided 1 cm proximal to the reservoir and secured to the uncapped collar of a plastic water bottle using a rubber band.

External stoma diversion; this image shows the external stoma diversion as applied in the patient setting.
DISCUSSION
Considerations of external stoma diversion
Patient selection
This procedure was performed on a 63-year-old male with a complicated abdominal surgical history, requiring three laparotomies and resulting in an end ileostomy. The patient had consistent, copious output from his ostomy and was managing output using cloth for absorption. This led to painful maceration (Fig. 3) of the peristomal skin that was not responsive to standard measures (e.g. ostomy paste, traditional stoma appliances, stool bulkers). The patient subsequently experienced significant weight loss due to reduced oral intake. Therefore, after obtaining informed consent from the patient and family, the external stoma diversion was offered as a palliative measure.
Expertise required for the performance and care of the external stoma diversion
External stoma diversion can be performed in the operating room, at the bedside, or in the clinic depending on practitioner preference and patient comfort. It is performed using local anesthesia and does not require an anesthesia provider. It can be placed by a surgeon, general practitioner or surgical non-physician clinician. For this patient at postprocedure day 7, the proximal aspect of the condom becomes torn at the suture site, necessitating removal. Though at this stage of healing, the surrounding skin was improved and could accommodate traditional stoma bags, the patient and his family requested that the local general practitioner remove and replace the external stoma diversion using the same technique (Fig. 4).

Improved peristomal wound; on postoperative day 7 the external stoma diversion was removed; significant improvement of peristomal skin maceration is noted.
Duration of treatment and finances
The external stoma diversion is intended to be a temporary, palliative measure due to theoretical potential suture erosion through peristomal skin and need for removal or replacement of the device. The patient had the external stoma diversion removed on postprocedural day 7 with significant improvement of peristomal skin maceration and without any procedure-related complications (Fig. 4). In our experience, the device remained functional for 7 days due to eventual tearing of the thin condom material. It is possible that a longer duration of application may be achieved using sturdier material.
CONCLUSION
The facilitation of access to safe, timely and affordable surgical care requires consideration of new surgical techniques to mitigate and palliate disease processes that have progressed beyond standard treatments. Often, intestinal stoma care and complications are a challenge in resource-limited settings due to limited healthcare access, high cost of ostomy supplies and availability of wound care services. Surgeons must, therefore, be prepared to address stomal complications and provide patients with guidance on ostomy care. The external stoma diversion is a palliative procedure in the armament of the general surgeon that assists with peristomal wound healing and can improve a patient’s quality of life.
DISCLOSURES
The authors have no disclosures related to the content of this article and no conflicts of interest.
ETHICAL APPROVAL
We have reported a single case, not a clinical study, with no requirement for ethical approval. The patient provided consent for the discussion of his case in a deidentified fashion.
FUNDING
None.
CONFLICT OF INTEREST STATEMENT
None declared.



